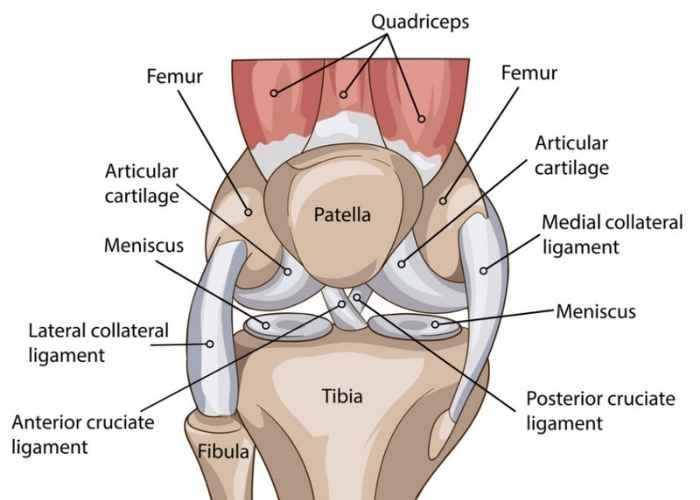
Knee Anatomy
The knee is a complex joint made up of bones, tendons, ligaments, and muscles, all working together to ensure proper function and stability during movement. It primarily consists of the femur (thighbone) and tibia (shinbone), with the patella (kneecap) protecting the joint. Articular cartilage covers the bone surfaces to reduce friction, while the menisci act as shock absorbers. Ligaments, including the medial and lateral collateral ligaments and the anterior and posterior cruciate ligaments, provide stability. Major muscle groups, like the quadriceps and hamstrings, facilitate knee movement through their associated tendons.
Conditions & Treatments
Knee Arthritis: Causes, Types, and Symptoms
Knee arthritis is a condition where the cartilage in the knee joint breaks down, leading to pain, stiffness, and limited mobility. It can significantly impact daily activities such as walking, climbing stairs, or standing for long periods.
Causes of Knee Arthritis
The causes of knee arthritis can vary, but common factors include:
- Osteoarthritis (OA): The most common form of knee arthritis, caused by the gradual wear and tear of cartilage over time, often associated with aging or joint overuse.
- Rheumatoid Arthritis (RA): An autoimmune condition that causes chronic inflammation in the knee joint, leading to pain, swelling, and possible joint damage.
- Post-Traumatic Arthritis: Develops after an injury, such as a knee fracture or ligament tear, that disrupts the integrity of the knee joint and leads to arthritis over time.
- Infectious Arthritis: Caused by an infection in the knee joint, leading to inflammation, swelling, and pain.
Types of Knee Arthritis
- Osteoarthritis (OA): The most common form of knee arthritis, often affecting older adults. It involves the gradual loss of cartilage, resulting in bone-on-bone contact and pain.
- Rheumatoid Arthritis (RA): An autoimmune disorder that causes inflammation in the synovium of the knee joint, often leading to pain, swelling, and deformity.
- Post-Traumatic Arthritis: A form of arthritis that occurs after a significant knee injury or trauma, causing damage to the cartilage and accelerating the degeneration of the joint.
- Infectious Arthritis: Rare but serious, this type of arthritis occurs when bacteria or viruses infect the knee joint, leading to inflammation and severe pain.
Symptoms of Knee Arthritis
- Pain: Pain in the knee, especially with movement, weight-bearing activities, or prolonged sitting.
- Stiffness: Limited range of motion, particularly after rest or in the morning.
- Swelling: Inflammation and puffiness around the knee joint, often causing discomfort.
- Instability: A feeling of weakness or giving way in the knee, especially with standing or walking.
- Crepitus: A sensation of grinding, popping, or crackling in the knee joint during movement.
Knee arthritis can significantly affect quality of life, but treatment options such as physical therapy, medications, injections, or in severe cases, knee replacement surgery, can help reduce pain and improve function.
Treatments
Bursitis: Causes, Types, and Symptoms
Bursitis is the inflammation of a bursa, a small, fluid-filled sac that acts as a cushion between bones and soft tissues like muscles and tendons. When a bursa becomes irritated or inflamed, it can cause pain and swelling, making movement difficult.
Causes of Bursitis
Bursitis often results from repetitive motion, prolonged pressure, or injury to the affected area. Common causes include:
- Repetitive Movements: Activities that involve repetitive motion, such as sports or manual labor, can lead to bursitis.
- Trauma or Injury: A direct blow or injury to a joint can cause inflammation in the bursa.
- Overuse: Excessive use of certain joints, especially in positions that put pressure on the bursa, can lead to irritation.
- Infection: In rare cases, a bacterial infection can cause septic bursitis, leading to more severe symptoms.
- Medical Conditions: Conditions like rheumatoid arthritis, gout, or diabetes can increase the risk of developing bursitis.
Common Types of Bursitis
- Shoulder Bursitis: Inflammation of the bursa in the shoulder, often caused by repetitive overhead movements.
- Elbow Bursitis: Also known as “student’s elbow,” it occurs when the bursa at the tip of the elbow becomes inflamed, typically from prolonged pressure or frequent leaning.
- Hip Bursitis: Inflammation of the bursa in the hip, often caused by repetitive movements or long periods of sitting.
- Knee Bursitis: Common in athletes or individuals who kneel frequently, this condition affects the bursa in the knee joint.
Symptoms of Bursitis
- Pain: Aching or sharp pain in the affected joint, often aggravated by movement or pressure.
- Swelling: Visible swelling around the affected joint.
- Tenderness: The area around the bursa may be sensitive to touch.
- Stiffness: Limited range of motion in the affected joint.
- Redness and Warmth: In the case of infection, the skin may appear red and feel warm to the touch.
Bursitis can significantly affect daily activities, but treatment options such as rest, ice, anti-inflammatory medications, physical therapy, or in more severe cases, injections or surgery, can help alleviate symptoms.
Treatments
Ligament Sprains: Causes, Types, and Symptoms
A ligament sprain is an injury to the tough, fibrous tissue that connects bones together and stabilizes joints. Ligament sprains can range from mild to severe, often causing pain, swelling, and difficulty moving the affected joint.
Causes of Ligament Sprains
Ligament sprains typically occur when a joint is forced beyond its normal range of motion. Common causes include:
- Trauma: A sudden impact or forceful movement, such as a fall, car accident, or sports-related injury, can overstretch or tear ligaments.
- Twisting or Overextending: Activities that involve rapid twisting motions, such as twisting an ankle or knee, can lead to sprains.
- Repetitive Stress: Overuse or repetitive strain on a joint, such as during sports or strenuous physical activities, can weaken ligaments and make them more prone to injury.
Types of Ligament Sprains
Ligament sprains are classified into three grades based on the severity of the injury:
- Grade 1 (Mild): A mild sprain occurs when the ligament is stretched but not torn. This usually causes mild pain, swelling, and minimal joint instability.
- Grade 2 (Moderate): A moderate sprain involves partial tearing of the ligament, leading to more significant pain, swelling, bruising, and some instability in the joint.
- Grade 3 (Severe): A severe sprain is a complete tear or rupture of the ligament, resulting in intense pain, swelling, bruising, and significant joint instability or immobility.
Common Areas Affected by Ligament Sprains
- Ankle: One of the most common sprains, typically caused by rolling or twisting the ankle.
- Knee: Sprains to ligaments such as the ACL (anterior cruciate ligament) or MCL (medial collateral ligament) often occur during sports or physical activities.
- Wrist: Ligament sprains in the wrist can occur from falls or direct trauma.
- Thumb: Sprains in the thumb are common in contact sports or activities requiring gripping.
Symptoms of Ligament Sprains
- Pain: Localized pain in the affected joint, which may increase with movement.
- Swelling: Inflammation around the joint, making it tender to touch.
- Bruising: Discoloration due to blood pooling under the skin.
- Instability: The feeling that the joint may give way or lack strength, especially in severe sprains.
- Limited Mobility: Difficulty moving the joint due to pain or stiffness.
Treatment for ligament sprains depends on the severity of the injury and may include physical therapy, medications for pain management, and in more severe cases, surgical intervention.
Treatments
Meniscus Injuries/Tears: Causes, Types, and Symptoms
The meniscus is a C-shaped cartilage in the knee that acts as a cushion and stabilizer between the femur and tibia. Meniscus tears are common knee injuries, often caused by twisting motions, impact, or degeneration over time. These injuries can lead to pain, swelling, and limited knee function.
Causes of Meniscus Injuries/Tears
Meniscus tears often occur due to:
- Twisting or Pivoting: Sudden turns or twisting movements, especially during sports, can tear the meniscus.
- Trauma or Impact: Direct blows or falls on the knee, such as during contact sports or accidents, can damage the meniscus.
- Degeneration: Over time, the meniscus can weaken and become more prone to tears, especially in older adults.
Types of Meniscus Tears
Meniscus tears are classified based on their location and shape:
- Horizontal Tear: A tear along the top and bottom of the meniscus, which may cause the meniscus to split into two parts.
- Vertical Tear: A tear that runs vertically, often along the outer edge of the meniscus.
- Radial Tear: A tear that radiates outward from the center of the meniscus, often causing significant instability in the knee.
- Complex Tear: A combination of several types of tears, leading to more severe damage and symptoms.
Symptoms of Meniscus Tears
- Pain: Pain in the knee, especially when twisting or rotating the leg.
- Swelling: Inflammation around the knee joint, often occurring within a few hours of the injury.
- Limited Range of Motion: Difficulty bending or straightening the knee due to pain or mechanical blockages.
- Instability: A feeling that the knee might give way or buckle during movement.
- Popping or Clicking Sensation: A popping sound or sensation in the knee during movement.
Treatment for meniscus tears depends on the severity and type of tear and may include physical therapy, rest, anti-inflammatory medications, or, in more severe cases, surgery.
Treatments
Tendonitis and Tendinosis: Causes, Types, and Symptoms
Tendonitis and tendinosis are conditions that involve inflammation or degeneration of tendons, the thick cords that attach muscles to bones. These conditions can cause significant pain and limit movement, often affecting active individuals or those engaged in repetitive motions.
Common Types of Tendonitis and Tendinosis
Tendonitis
Tendonitis is the inflammation of a tendon, often caused by overuse, injury, or repetitive stress. It typically occurs in the shoulder, elbow, wrist, knee, or Achilles tendon. Inflammation can make the tendon swollen, painful, and less flexible. Common types include:
- Rotator Cuff Tendonitis (shoulder)
- Tennis Elbow (lateral epicondylitis, elbow)
- Achilles Tendonitis (ankle)
- Patellar Tendonitis (knee)
Tendinosis
Tendinosis is the degeneration of a tendon’s collagen due to chronic overuse, without the inflammation seen in tendonitis. This leads to weakened tendons, increasing the risk of further injury. It most often affects tendons in the:
- Elbow (lateral epicondylitis or “tennis elbow”)
- Knee (patellar tendon)
- Shoulder (rotator cuff tendons)
Symptoms of Tendonitis and Tendinosis
- Pain: Localized pain at the site of the tendon, often worsened by movement or activity.
- Swelling: Tenderness and visible swelling around the affected tendon.
- Stiffness: Reduced range of motion in the joint or muscle.
- Weakness: Difficulty using the affected limb due to pain or discomfort.
- Crepitus: A sensation of grating or crackling during movement.
Tendonitis and tendinosis can significantly impact quality of life, particularly for individuals who rely on repetitive motions. Early diagnosis and treatment, including rest, physical therapy, medications, injections, or surgery, can help manage symptoms and promote recovery.
Treatments
Bone Contusions to the Knee: Causes, Types, and Symptoms
A bone contusion, or bone bruise, is an injury to the bone that causes localized swelling, pain, and bruising. Bone contusions to the knee typically occur due to trauma or impact, such as from a fall, sports injury, or direct blow to the knee. While not as severe as a fracture, bone contusions can still result in significant pain and limited mobility.
Causes of Bone Contusions to the Knee
Bone contusions in the knee are commonly caused by:
- Direct Trauma: A direct blow to the knee, such as during contact sports (football, basketball) or from a fall, can cause a bone bruise.
- Overuse or Repetitive Stress: Repeated stress or strain on the knee, especially in high-impact activities, may contribute to bone contusions.
- Twisting or Rotational Movements: Sudden twisting or pivoting motions can lead to a bone bruise in the knee, especially if there is direct force involved.
Types of Bone Contusions in the Knee
- Superficial Contusion: A mild bone bruise affecting the surface of the bone, often leading to localized swelling and discomfort.
- Deep Contusion: A more severe bruise that penetrates deeper into the bone, often resulting in more significant pain, swelling, and longer recovery time.
- Bone Marrow Edema: This refers to fluid buildup within the bone tissue, typically seen in more severe contusions. It can cause significant pain and may take longer to heal.
Symptoms of Bone Contusions to the Knee
- Pain: Deep, aching pain at the site of the contusion, often aggravated by movement or pressure.
- Swelling: Noticeable swelling around the knee joint, which may develop quickly after the injury.
- Bruising: Discoloration of the skin due to blood accumulation under the skin, often appearing in a blue or purple color.
- Limited Range of Motion: Difficulty moving the knee due to pain or swelling.
- Tenderness: Increased sensitivity to touch around the injured area.
Treatment for bone contusions typically includes rest, ice, and elevation to reduce swelling and promote healing. Depending on the severity, physical therapy may also be recommended to restore knee function.
Treatments
Strains: Causes, Types, and Symptoms
A strain is an injury to a muscle or tendon (the tissue that connects muscles to bones), caused by overstretching or tearing. Strains can range from mild to severe and typically result from overuse, improper movement, or sudden forceful actions. They often affect the back, hamstrings, and other muscles throughout the body, causing pain and limiting mobility.
Causes of Strains
Strains commonly occur due to:
- Overuse or Repetitive Motion: Continuous or excessive use of a muscle without proper rest can lead to strain, especially in athletes or individuals with physically demanding jobs.
- Sudden or Forceful Movements: Lifting heavy objects, twisting motions, or explosive actions (such as sprinting or jumping) can strain muscles or tendons.
- Poor Flexibility or Warm-Up: Lack of proper stretching or warm-up before physical activity increases the risk of muscle strains.
Types of Strains
Strains are typically classified into three grades based on severity:
- Grade 1 (Mild): A mild strain involves overstretching or slight tearing of the muscle or tendon fibers, causing minimal pain, swelling, and no significant loss of function.
- Grade 2 (Moderate): A moderate strain involves partial tearing of muscle fibers, leading to moderate pain, swelling, and some loss of strength or movement.
- Grade 3 (Severe): A severe strain refers to a complete tear of the muscle or tendon, often causing intense pain, significant swelling, bruising, and a noticeable loss of function or stability.
Symptoms of Strains
- Pain: Sharp or aching pain in the affected muscle, which may worsen with movement or activity.
- Swelling: Inflammation or puffiness around the injured muscle or tendon.
- Bruising: Discoloration from blood accumulating beneath the skin.
- Limited Range of Motion: Difficulty moving the affected area due to pain or weakness.
- Weakness: A feeling of instability or weakness in the muscle, making it hard to perform usual movements or activities.
Treatment for strains typically includes rest, ice, compression, and elevation (R.I.C.E.), along with stretching and strengthening exercises to aid in recovery. Severe strains may require medical intervention, including physical therapy or, in some cases, surgery.
Treatments
Fractures: Causes, Types, and Symptoms
A fracture refers to a break in a bone, which can result from trauma, stress, or certain medical conditions. Fractures can occur in any bone and vary in severity, often leading to pain, swelling, and difficulty moving the affected area.
Common Types of Fractures
Closed Fracture
A closed fracture occurs when the bone breaks but does not pierce the skin. These fractures can range from simple cracks to complete breaks, typically resulting from falls, accidents, or direct trauma.
Open Fracture
An open fracture, or compound fracture, happens when the bone breaks and punctures the skin. These fractures are more severe, often requiring surgical intervention to prevent infection and properly align the bone.
Stress Fracture
A stress fracture is a small, hairline crack caused by repetitive pressure or overuse, often seen in athletes or individuals engaging in high-impact activities.
Symptoms of a Fracture
- Pain: Sudden, sharp pain at the site of the fracture.
- Swelling: Inflammation around the injured area.
- Bruising: Discoloration and tenderness.
- Deformity: Visible misalignment or unnatural positioning of the bone.
- Limited Movement: Difficulty moving the affected limb or joint.
Fractures vary in severity and treatment, with some requiring cast immobilization, while others may need surgical intervention. Prompt medical attention is crucial for proper diagnosis and recovery. If you suspect a fracture, contact an orthopedic specialist for evaluation and care.
Treatments
Osteochondral Defects of the Knee: Causes, Types, and Symptoms
Osteochondral defects in the knee refer to damage to both the articular cartilage and the underlying bone. This type of injury can occur due to trauma, overuse, or degenerative conditions, leading to pain, swelling, and difficulty moving the knee joint. These defects can disrupt the smooth movement of the knee and often impact daily activities and athletic performance.
Causes of Osteochondral Defects in the Knee
Osteochondral defects are commonly caused by:
- Trauma or Injury: Direct impact or injury to the knee, such as from a fall, car accident, or sports-related trauma, can lead to osteochondral damage.
- Repetitive Stress: Overuse or repetitive motion of the knee, particularly in athletes or individuals with physically demanding jobs, can gradually wear down the cartilage and underlying bone.
- Degenerative Conditions: Conditions like osteoarthritis can lead to the breakdown of both cartilage and bone, resulting in osteochondral defects.
- Previous Knee Injuries: Previous knee injuries, such as ligament or meniscus tears, can increase the risk of developing osteochondral defects.
Types of Osteochondral Defects in the Knee
- Grade 1: Minor damage to the cartilage without involvement of the underlying bone. Symptoms may be mild, and healing is often possible with conservative treatment.
- Grade 2: Moderate cartilage damage with some involvement of the underlying bone. Symptoms may include pain, swelling, and decreased range of motion.
- Grade 3: Severe damage to both cartilage and bone, often resulting in significant pain, joint instability, and difficulty walking or participating in physical activity.
- Grade 4: The most severe form, where both cartilage and bone are significantly damaged or lost. This stage may require surgical intervention to restore knee function.
Symptoms of Osteochondral Defects in the Knee
- Pain: A deep, aching pain in the knee, which often worsens with physical activity or after long periods of weight-bearing.
- Swelling: Inflammation around the knee joint, which can appear shortly after an injury or after extended use.
- Limited Range of Motion: Difficulty bending or straightening the knee due to pain or mechanical blocking.
- Instability: A feeling that the knee may give way, especially when walking or performing weight-bearing activities.
- Grinding or Locking: A sensation of grinding or locking in the knee, particularly when the joint moves.
Treatment for osteochondral defects typically involves conservative measures such as physical therapy, pain management, and rest. In more severe cases, surgical options like microfracture, osteochondral grafting, or cartilage replacement procedures may be considered to repair or restore the damaged cartilage and bone.
Treatments
IT Band Friction Syndrome
Iliotibial (IT) band friction syndrome is a common condition that causes pain on the outside of the knee or hip, often experienced by runners, cyclists, or individuals who engage in repetitive lower body movements. This condition occurs when the IT band, a thick band of tissue running down the outside of the thigh from the hip to the knee, becomes tight or irritated, rubbing against the bones of the knee joint.
What Is IT Band Friction Syndrome?
The IT band is a strong fibrous tissue that helps stabilize the knee during movement. In IT band friction syndrome, repeated friction between the IT band and the outer part of the knee leads to inflammation and pain. The condition is often associated with overuse, improper biomechanics, or muscle imbalances that cause the IT band to become tight and irritated.
Causes of IT Band Friction Syndrome
- Overuse: Repetitive activities such as running, cycling, or hiking, especially on uneven terrain or long distances, can stress the IT band.
- Muscle Imbalances: Weak hip abductors or tight quadriceps can alter the way the IT band moves, increasing friction on the knee joint.
- Poor Biomechanics: Abnormalities in walking or running form, such as overpronation or an improper stride, can contribute to the condition.
- Inflexibility: Lack of flexibility in the hips, knees, or IT band itself can make it more prone to irritation.
Symptoms of IT Band Friction Syndrome
- Pain on the Outer Knee: A sharp or burning pain on the outside of the knee, often worsened by activities like running, cycling, or descending stairs.
- Pain that Worsens with Activity: The pain may start mild but can intensify with prolonged use of the affected leg or after activity.
- Swelling or Tenderness: Swelling may occur along the outside of the knee, and the area may be tender to the touch.
- Decreased Range of Motion: Difficulty bending or straightening the knee due to discomfort.
Treatment for IT Band Friction Syndrome
Treatment for IT band friction syndrome focuses on reducing inflammation, improving flexibility, and addressing the underlying causes of the condition. Initial treatments include rest, ice, and anti-inflammatory medications. Stretching and strengthening exercises, particularly for the hip and thigh muscles, can help relieve tension in the IT band. Physical therapy may also help improve biomechanics and prevent recurrence. In rare cases, if conservative treatments do not provide relief, corticosteroid injections or surgery may be considered.
If you’re experiencing pain or discomfort on the outside of your knee or hip, especially after physical activity, it’s important to consult with an orthopedic specialist to assess your condition and explore the most effective treatment options.
Treatments
Steroid Injections
What Are Steroid Injections?
These injections usually contain corticosteroids, which are powerful anti-inflammatory medications. They help reduce swelling and pain quickly and are often mixed with a local anesthetic for added relief.
When Are They Used?
Steroid injections are commonly used for:
- Arthritis: They can ease pain in joints affected by osteoarthritis or rheumatoid arthritis.
- Tendinitis: Conditions like tennis elbow or Achilles tendinitis respond well to these injections.
- Bursitis: Inflammation in the bursae, which cushion your joints, can be treated effectively.
- Joint Injuries: They’re helpful for both acute injuries and ongoing pain from conditions like ligament tears.
Benefits
- Quick Pain Relief: Many people feel better within days.
- Less Need for Oral Medications: This can help you avoid the side effects of taking pills.
- Improved Mobility: You may be able to get back to your normal activities more easily.
Risks to Consider
While steroid injections can be very effective, they’re not without risks:
- Injection Site Pain: You might feel some discomfort right after the injection.
- Infection: Though rare, there’s a slight chance of infection.
- Tissue Damage: Frequent injections can harm nearby tissues, including tendons and cartilage.
- Wider Effects: Corticosteroids can affect your whole body, possibly raising blood sugar or impacting hormone levels.
How Often Can You Get Them?
Typically, doctors recommend limiting steroid injections to about three times a year for the same joint to avoid complications.
Viscosupplementation - Knee
Viscosupplementation for Knee Osteoarthritis: Uses, Benefits, and Risks
Viscosupplementation is a treatment option for knee osteoarthritis (OA) that involves injecting a gel-like substance into the knee joint to help improve mobility and reduce pain. The injection aims to mimic the natural synovial fluid that lubricates the joint, offering relief from the symptoms of OA.
What Is Viscosupplementation?
Viscosupplementation involves injecting hyaluronic acid, a substance naturally found in the synovial fluid of healthy joints, into the knee. This treatment helps to restore the joint’s natural lubrication, reduce friction, and relieve pain and stiffness associated with knee OA. Hyaluronic acid injections can be given as a series of injections over a few weeks or as a single injection, depending on the product and the patient’s condition.
When Is Viscosupplementation Used?
Viscosupplementation is primarily used for patients with knee osteoarthritis who have not found sufficient relief from other treatments, such as physical therapy, anti-inflammatory medications, or oral pain relievers. It is typically recommended for:
- Knee Osteoarthritis: Viscosupplementation is commonly used to treat moderate to severe OA in the knee, particularly when conservative treatments are no longer effective.
- Pain Management: For patients seeking to manage chronic knee pain, this treatment can be an alternative to corticosteroid injections or for those who wish to avoid the side effects of oral pain medications.
- Post-Surgical Recovery: It may be used in combination with other treatments to support recovery following knee surgery or to delay the need for more invasive procedures, such as joint replacement.
Benefits of Viscosupplementation
- Pain Relief: Many patients experience a reduction in knee pain, allowing them to engage in daily activities with less discomfort.
- Improved Mobility: By restoring lubrication and reducing friction in the knee, viscosupplementation can enhance joint function and improve range of motion.
- Minimized Need for Oral Medications: Viscosupplementation offers an alternative to oral pain medications or corticosteroid injections, potentially reducing the need for long-term drug use.
- Fewer Side Effects: Compared to corticosteroids, hyaluronic acid injections typically have fewer side effects and can be used repeatedly over time.
Risks to Consider
While viscosupplementation is generally considered safe, there are some potential risks to be aware of:
- Injection Site Reactions: Some individuals may experience mild pain, swelling, or redness at the injection site following the procedure.
- Infection: Although rare, there is a small risk of infection at the injection site.
- Temporary Pain or Stiffness: Some patients may experience an increase in pain or stiffness in the knee shortly after the injection, which typically resolves within a few days.
- Not a Cure: Viscosupplementation is not a cure for knee osteoarthritis, and its effects are temporary, meaning repeated injections may be necessary for ongoing symptom relief.
How Often Can You Get Viscosupplementation?
The frequency of viscosupplementation injections depends on the specific product used and the patient’s response to treatment. In most cases, a series of injections is given over a period of several weeks, though some newer formulations allow for a single injection. Typically, injections may be repeated every six months to a year, based on individual needs and symptoms.
Viscosupplementation can be an effective treatment for knee osteoarthritis, offering pain relief and improved function for those who have not found success with other treatments.
Zilretta - Knee
Zilretta (Slow-Release Kenalog Injection) for Knee Osteoarthritis: Uses, Benefits, and Risks
Zilretta is an advanced treatment for knee osteoarthritis (OA) that provides long-lasting pain relief through a slow-release corticosteroid injection. It is designed to deliver anti-inflammatory effects over an extended period, helping to manage knee OA symptoms and improve mobility.
What Is Zilretta?
Zilretta is a formulation of triamcinolone acetonide, a corticosteroid, that is injected into the knee joint. Unlike traditional steroid injections, Zilretta is designed for slow release, providing continuous relief over the course of several months. This sustained effect helps reduce inflammation and pain associated with knee OA, offering longer-lasting benefits compared to conventional steroid injections.
When Is Zilretta Used?
Zilretta is typically used for individuals with knee osteoarthritis who have not found sufficient relief from other treatments, such as physical therapy, oral pain medications, or other injections. It is particularly effective for:
- Knee Osteoarthritis: Zilretta is used to manage moderate to severe knee OA, especially when other treatments have been ineffective.
- Pain Management: It offers long-lasting relief from pain, which can help individuals engage in daily activities and improve mobility.
- Alternative to Oral Medications: Zilretta can be an effective option for those looking to reduce their reliance on oral pain medications, such as NSAIDs, which may have long-term side effects.
Benefits of Zilretta
- Extended Pain Relief: Zilretta provides long-lasting relief by slowly releasing corticosteroid medication over the course of several months, reducing the need for frequent injections.
- Improved Mobility: Many patients experience improved knee function, allowing them to move more freely and engage in everyday activities with less discomfort.
- Targeted Treatment: The slow-release mechanism allows Zilretta to directly target inflammation in the knee joint, providing effective pain relief.
- Reduced Need for Oral Medications: By offering extended relief from pain, Zilretta reduces the need for oral pain medications, helping to avoid their potential side effects.
Risks to Consider
While Zilretta is a generally safe and effective treatment for knee OA, there are some risks to be aware of:
- Injection Site Reactions: Some patients may experience mild pain, swelling, or redness at the injection site after the procedure.
- Infection: Though rare, there is a small risk of infection at the injection site.
- Temporary Pain Increase: In some cases, patients may experience temporary pain or discomfort shortly after the injection, which typically resolves within a few days.
- Not a Cure: While Zilretta can offer significant pain relief, it is not a cure for knee osteoarthritis, and its effects are temporary. Repeat injections may be needed for ongoing symptom management.
How Often Can You Get Zilretta?
Typically, Zilretta injections are administered once every three months. The exact frequency may vary depending on the severity of symptoms and the patient’s response to the treatment. Your orthopedic specialist will help determine the appropriate schedule based on your condition and overall health.
Zilretta can be a highly effective option for managing knee osteoarthritis, providing long-term relief from pain and improving joint function.
iovera°
iovera° for Knee Osteoarthritis: Uses, Benefits, and Risks
iovera° is a cutting-edge treatment for knee osteoarthritis (OA) that uses cryoneurolysis (a technique involving cold therapy) to target and freeze the nerves responsible for pain, offering significant relief without the need for injections of steroids or other medications.
What Is iovera°?
iovera° is a non-invasive procedure that involves the application of cold to the nerves around the knee joint to temporarily disrupt pain signals. Using a specialized device, a small probe is applied to the skin near the knee, delivering precise, controlled freezing temperatures to the sensory nerves that transmit pain signals from the joint. This process temporarily “turns off” the pain signals, providing pain relief without medication or surgery.
When Is iovera° Used?
iovera° is typically used for individuals with knee osteoarthritis who are seeking an alternative to more traditional treatments like steroid injections or pain medications. It is effective for:
- Knee Osteoarthritis: iovera° is commonly used to manage chronic knee pain associated with moderate to severe knee OA.
- Pain Management: Ideal for individuals who are looking for a non-pharmacologic option to reduce pain and improve mobility.
- Pre-surgical Pain Relief: iovera° can also be used to manage pain before knee surgery or as a bridge treatment for patients who wish to delay surgery.
Benefits of iovera°
- Non-invasive Treatment: iovera° is a non-surgical, non-medication option for knee OA pain relief, making it ideal for patients looking to avoid the side effects of drugs or the risks of surgery.
- Rapid Pain Relief: Many patients experience immediate relief after the procedure, with benefits that can last for several months.
- Long-lasting Effect: The pain-relief effects typically last up to 3 months, after which the procedure can be repeated as needed.
- Minimal Downtime: Since there are no incisions or medications involved, patients can resume normal activities shortly after treatment.
- Fewer Side Effects: Unlike medications or injections, iovera° does not carry the risk of systemic side effects, such as those associated with steroids or oral pain relievers.
Risks to Consider
Although iovera° is generally considered safe, there are some potential risks to keep in mind:
- Temporary Sensitivity: Some patients may experience temporary sensitivity or discomfort at the treatment site following the procedure.
- Localized Skin Reactions: There may be mild redness, swelling, or bruising in the area where the cold therapy was applied, which usually resolves quickly.
- Not a Cure: iovera° provides temporary pain relief, and its effects typically last for several months. Repeated treatments may be necessary to maintain relief.
How Often Can You Get iovera°?
The iovera° procedure typically provides pain relief for up to 3 months. Depending on the severity of symptoms, treatment can be repeated every few months, as necessary. Your orthopedic specialist will assess your progress and determine the optimal schedule for further treatments.
iovera° is an innovative, non-invasive option for knee osteoarthritis pain relief, offering an alternative to medications and surgery.
Other Injections - Knee
Toradol Injections for Osteoarthritis: Uses, Benefits, and Risks
Intra-articular Toradol injections are a treatment option for knee osteoarthritis (OA) that provides effective, short-term pain relief. Toradol (ketorolac) is a nonsteroidal anti-inflammatory drug (NSAID) commonly used to reduce pain and inflammation, and when injected directly into the knee joint, it can target inflammation at the source, offering relief from the symptoms of OA.
What Are Intra-Articular Knee Toradol Injections?
Intra-articular Toradol injections involve the direct injection of Toradol into the knee joint. As a potent NSAID, Toradol works by inhibiting the production of inflammatory chemicals in the body, specifically prostaglandins, which contribute to pain and swelling in the joint. When injected directly into the knee, Toradol offers targeted, localized pain relief by addressing inflammation in the joint space.
When Are They Used?
Intra-articular Toradol injections are primarily used for individuals suffering from knee osteoarthritis who are seeking relief from pain and inflammation. They are often considered for:
- Knee Osteoarthritis: Toradol injections are used to manage moderate to severe knee OA pain, particularly in cases where oral NSAIDs or other conservative treatments have been ineffective.
- Short-term Pain Relief: This injection is ideal for patients who need temporary pain relief to improve mobility and function, allowing them to engage in daily activities.
- Alternative to Steroid Injections: Toradol injections may be considered for those who wish to avoid corticosteroid injections, offering a different mechanism of action with fewer long-term risks.
Benefits of Intra-Articular Toradol Injections
- Effective Pain Relief: Toradol is a strong anti-inflammatory medication, offering significant relief from knee pain and inflammation in patients with OA.
- Targeted Treatment: By delivering the medication directly into the knee joint, the treatment addresses the source of the pain, providing faster and more focused relief compared to oral NSAIDs.
- Reduced Need for Oral Medications: Intra-articular Toradol injections can help reduce reliance on oral NSAIDs, which may have side effects when used long-term.
- Quick Onset of Action: Many patients experience pain relief soon after the injection, with effects that can last for several weeks.
Risks to Consider
While intra-articular Toradol injections are generally well-tolerated, there are some risks to consider:
- Injection Site Pain: Some discomfort or swelling at the injection site may occur immediately following the procedure.
- Infection: As with any injection, there is a small risk of infection at the injection site.
- Gastrointestinal Issues: Although less common with intra-articular use, Toradol may still cause gastrointestinal issues, including ulcers or bleeding, especially in individuals with a history of stomach problems.
- Kidney Function: NSAIDs like Toradol can affect kidney function, so caution is required for patients with existing kidney issues.
How Often Can You Get Intra-Articular Toradol Injections?
Intra-articular Toradol injections are typically administered every few weeks, depending on the severity of symptoms and how well the patient responds to the treatment. However, due to the potential for side effects with prolonged use, it is generally recommended to limit the number of injections per year. Your orthopedic specialist will determine the appropriate frequency of injections based on your individual condition.
Intra-articular Toradol injections can provide effective, short-term relief from knee osteoarthritis pain, offering a non-steroidal alternative to corticosteroid injections.
Platelet Rich Plasma Therapy
Platelet-Rich Plasma (PRP) Injections for Knee Osteoarthritis: Uses, Benefits, and Risks
Platelet-rich plasma (PRP) injections are an innovative treatment for knee osteoarthritis (OA) that uses the body’s own healing properties to reduce pain and improve function. PRP therapy involves extracting a sample of the patient’s blood, concentrating the platelets, and injecting the enriched plasma directly into the affected joint to stimulate healing and reduce inflammation.
What Are PRP Injections?
PRP injections involve drawing a small amount of the patient’s blood, processing it in a centrifuge to concentrate the platelets, and then injecting this platelet-rich plasma into the knee joint. Platelets contain growth factors and proteins that play a key role in tissue repair and inflammation reduction. By injecting concentrated platelets directly into the joint, PRP therapy helps promote healing, reduce inflammation, and alleviate pain caused by knee OA.
When Are PRP Injections Used?
PRP injections are primarily used for patients with knee osteoarthritis who are seeking a non-surgical solution to manage pain and improve joint function. PRP therapy is often considered for:
- Knee Osteoarthritis: PRP injections are used to manage moderate to severe knee OA pain, especially in patients who are not candidates for surgery or who want to avoid long-term use of pain medications.
- Joint Regeneration: PRP can help stimulate healing in damaged cartilage, potentially slowing the progression of osteoarthritis and improving joint health.
- Alternative to Steroid Injections: For patients who prefer to avoid corticosteroids, PRP offers a natural alternative with the potential for fewer side effects.
Benefits of PRP Injections
- Natural Healing: PRP injections utilize the body’s own healing factors, promoting tissue repair and regeneration within the knee joint.
- Reduced Pain and Inflammation: Many patients experience significant pain relief and reduced inflammation after PRP injections, leading to improved mobility.
- Non-Surgical Option: PRP therapy is a minimally invasive procedure that offers an alternative to knee surgery, providing potential relief without the risks and recovery time associated with surgery.
- Potential Long-term Benefits: Some patients may experience lasting relief, with continued improvements over several months, as the healing process continues.
Risks to Consider
Although PRP injections are generally considered safe, there are some risks to be aware of:
- Injection Site Discomfort: Some patients may experience mild pain, swelling, or redness at the injection site following the procedure.
- Temporary Pain Increase: In some cases, patients may notice a temporary increase in pain after the injection before improvement begins.
- Infection: Though rare, there is a slight risk of infection at the injection site.
- Not a Cure: PRP injections are not a cure for knee osteoarthritis, and their effectiveness may vary from patient to patient. Multiple injections may be needed for optimal results.
How Often Can You Get PRP Injections?
Typically, PRP injections are administered as a series of 1-3 treatments, spaced several weeks apart, depending on the severity of the osteoarthritis and the patient’s response to treatment. Your orthopedic specialist will assess your condition and determine the most appropriate treatment schedule.
PRP injections offer a promising, natural option for managing knee osteoarthritis by stimulating the body’s healing processes.
Orthobiologics
Orthobiologics for Joint Pain and Injuries: Uses and Benefits
Orthobiologics are a group of advanced treatments that harness the body’s natural healing abilities to address joint pain, injuries, and degenerative conditions. These treatments utilize biological materials derived from the patient’s own body to enhance recovery, reduce inflammation, and improve tissue repair without the need for surgery.
What Are Orthobiologics?
Orthobiologics include various therapies designed to accelerate healing and improve function. By using the body’s natural resources, these treatments can target damaged tissues, reduce pain, and help restore mobility.
When Are Orthobiologics Used?
Orthobiologics are commonly used for conditions like joint pain, tendon injuries, ligament damage, and early stages of osteoarthritis. They are ideal for patients looking to avoid more invasive treatments or surgery while still achieving effective, long-term results.
Benefits of Orthobiologics
- Natural Healing: These treatments stimulate the body’s natural repair processes to promote faster recovery.
- Minimally Invasive: Orthobiologic therapies are non-surgical, with minimal downtime.
- Targeted Treatment: These therapies directly address the injured area, offering localized relief.
- Reduced Risk of Side Effects: As these treatments often use your own body’s tissues, they carry a lower risk of complications compared to synthetic medications.
If you are considering orthobiologic treatments for joint or soft tissue injuries, consulting with an orthopedic specialist can help determine the right approach for your recovery.
Physical Therapy
Physical Therapy for Pain Relief and Rehabilitation: Benefits and Uses
Physical therapy is a treatment approach that focuses on improving movement, strength, and function through targeted exercises, manual therapy, and specialized techniques. It is an essential component of recovery for a variety of musculoskeletal conditions and injuries, helping patients regain mobility and reduce pain without the need for invasive treatments.
What Is Physical Therapy?
Physical therapy involves a personalized program of exercises and hands-on techniques designed to improve mobility, strengthen muscles, and alleviate pain. A licensed physical therapist evaluates each patient’s condition and develops a tailored plan to address specific needs, whether for recovery from surgery, injury, or managing chronic pain.
When Is Physical Therapy Used?
Physical therapy is commonly used for a variety of conditions, including:
- Post-Surgery Rehabilitation: It aids in regaining strength and mobility after orthopedic surgeries, such as joint replacements or ligament repairs.
- Sports Injuries: Physical therapy helps athletes recover from strains, sprains, and tendon injuries, improving strength and flexibility.
- Chronic Pain Management: Conditions like arthritis, back pain, and tendonitis can be managed effectively through physical therapy techniques.
- Injury Prevention: Physical therapy can be used proactively to strengthen muscles and improve movement patterns, reducing the risk of future injuries.
Benefits of Physical Therapy
- Pain Reduction: Targeted exercises and manual therapy techniques help alleviate pain by improving joint and muscle function.
- Improved Mobility: Physical therapy helps restore movement and flexibility, allowing patients to return to daily activities and sports.
- Strength and Stability: It improves muscle strength, which supports joints and reduces the risk of further injury.
- Non-Surgical Option: Physical therapy offers a non-invasive alternative to surgery, with long-term benefits for managing and recovering from musculoskeletal conditions.
If you are experiencing pain or limited movement, physical therapy can be an effective solution to help restore function and improve quality of life.
Arthroscopic Surgery - Knee
Knee Arthroscopic Surgery: A Minimally Invasive Solution for Knee Problems
Knee arthroscopic surgery is a minimally invasive procedure used to diagnose and treat a variety of knee issues. By utilizing small incisions and a tiny camera (arthroscope), orthopedic surgeons can view the inside of the knee joint and perform repairs with minimal disruption to surrounding tissues, promoting faster recovery and improved outcomes.
What Is Knee Arthroscopic Surgery?
Knee arthroscopic surgery involves making small incisions around the knee and inserting a camera to visualize the inside of the joint. Specialized instruments are then used to treat or repair damaged tissues, such as cartilage, ligaments, or meniscus. This technique minimizes the need for large incisions, reducing the trauma to healthy tissue and speeding up the recovery process.
When Is Knee Arthroscopic Surgery Used?
Knee arthroscopy is commonly used to treat a range of knee issues, including:
- Torn Cartilage or Meniscus: Arthroscopy can repair or remove damaged cartilage or meniscus, common in knee injuries.
- Ligament Injuries: Arthroscopic surgery is often used to repair torn ligaments, such as an ACL or MCL injury.
- Joint Debridement: For conditions like osteoarthritis, arthroscopy can remove bone fragments or damaged cartilage to alleviate pain and inflammation.
- Diagnosis: If other imaging tests are inconclusive, arthroscopy allows surgeons to directly assess the extent of damage in the knee.
Benefits of Knee Arthroscopic Surgery
- Minimally Invasive: The small incisions result in less damage to healthy tissue, leading to quicker recovery and reduced scarring.
- Shorter Recovery Time: Most patients experience less pain and are able to return to daily activities faster than with traditional open surgery.
- Lower Risk of Complications: With less disruption to the surrounding tissues, there is a lower risk of infection and other complications.
- Enhanced Precision: The clear, real-time visualization provided by the arthroscope allows surgeons to perform more accurate and effective treatments.
If you’re experiencing knee pain or injury, knee arthroscopic surgery offers a less invasive option to help diagnose, repair, and treat knee problems.
Robotic Assisted Total Knee Arthroplasty
Robotic-Assisted Total Knee Arthroplasty with the MAKO System: Precision in Knee Replacement Surgery
Robotic-assisted total knee arthroplasty (TKA) with the MAKO system is an advanced, minimally invasive procedure designed to improve the precision and outcomes of knee replacement surgery. Using state-of-the-art robotic technology, this system allows orthopedic surgeons to personalize the knee replacement process for each patient, ensuring a more accurate fit and alignment for long-term results.
What Is Robotic-Assisted Knee Surgery with the MAKO System?
The MAKO robotic system combines 3D imaging and real-time data to help guide the surgeon during the total knee replacement procedure. A pre-operative CT scan of the knee provides a detailed map of the joint, and the robotic arm helps the surgeon make precise cuts and adjustments to the bone and implant placement. This advanced technology allows for optimal alignment, which is critical for improving joint function and reducing wear on the implant.
When Is Robotic-Assisted Knee Surgery Used?
The MAKO system is typically used for patients with:
- Severe Osteoarthritis: For patients with advanced knee arthritis who experience pain, stiffness, and limited mobility.
- Deformities: To correct misalignment or deformities that may cause joint instability and uneven wear.
- Knee Joint Damage: For patients whose knee cartilage has been severely damaged due to trauma, injury, or degeneration.
Benefits of Robotic-Assisted Knee Surgery with the MAKO System
- Enhanced Precision: The robotic guidance ensures accurate implant placement and alignment, leading to better long-term function and durability of the knee replacement.
- Minimally Invasive: Smaller incisions are used, resulting in less tissue disruption, reduced scarring, and faster recovery.
- Customized Surgery: The 3D imaging and planning capabilities allow for a more personalized approach tailored to each patient’s unique anatomy.
- Faster Recovery: Many patients experience less pain and a quicker return to daily activities compared to traditional knee replacement surgery.
- Improved Outcomes: Studies have shown that robotic-assisted surgery can lead to more consistent outcomes, including better joint stability, alignment, and overall patient satisfaction.
If you are suffering from knee pain and considering knee replacement surgery, robotic-assisted TKA with the MAKO system offers an advanced, precise approach to improve your recovery and long-term outcomes.
Ultrasound-Guided Injections
Ultrasound-Guided Injections: Precision in Pain Management and Treatment
Ultrasound-guided injections are a minimally invasive procedure that uses real-time ultrasound imaging to guide the precise placement of injections into specific areas of the body. This technique enhances the accuracy of delivering medication, such as corticosteroids or hyaluronic acid, to joints, tendons, or soft tissues, improving the effectiveness of treatment for various musculoskeletal conditions.
What Are Ultrasound-Guided Injections?
During an ultrasound-guided injection procedure, a healthcare provider uses ultrasound imaging to visualize the targeted area and ensure that the injection is placed precisely where it is needed. This technique allows for better accuracy compared to traditional injections, ensuring that medication is delivered directly to the injured or inflamed tissue, increasing the likelihood of pain relief and healing.
When Are Ultrasound-Guided Injections Used?
Ultrasound-guided injections are commonly used to treat:
- Joint Inflammation: Such as in conditions like arthritis, where medication is injected directly into the joint to reduce pain and swelling.
- Tendinitis or Tendonitis: For conditions like tennis elbow or Achilles tendinitis, where medication is delivered to the affected tendon to relieve inflammation and pain.
- Bursitis: Inflammation in the bursa (fluid-filled sacs that cushion the joints) can be treated effectively with targeted injections.
- Soft Tissue Injuries: Injections can also be used for injuries to muscles, ligaments, and other soft tissues.
Benefits of Ultrasound-Guided Injections
- Precision: The use of real-time ultrasound ensures accurate injection placement, allowing for more effective treatment.
- Reduced Risk of Complications: The ability to visualize the injection site in real-time reduces the risk of accidentally injecting into the wrong area.
- Minimally Invasive: The procedure is quick, involves minimal discomfort, and typically requires no recovery time.
- Enhanced Treatment Effectiveness: With more accurate placement, ultrasound-guided injections provide better pain relief and faster healing.
Ultrasound-guided injections offer a targeted, effective approach to treating a variety of musculoskeletal conditions
Fracture Management
Fracture Management: A Comprehensive Approach to Bone Healing
Fractures are common injuries that occur when a bone is subjected to more force than it can handle, resulting in a break or crack. The management of fractures involves a careful, individualized approach to promote healing, restore function, and reduce the risk of complications.
What Is Fracture Management?
Fracture management encompasses a variety of techniques used to treat bone fractures and support the healing process. This can include non-surgical methods, such as immobilization with a cast or brace, as well as surgical interventions when necessary. The goal of treatment is to align the broken bones correctly, reduce pain, and allow for optimal recovery.
Treatment Options for Fractures
The management of fractures can involve:
- Conservative Treatment: For many fractures, especially those that are stable or non-displaced, conservative treatment such as casting or bracing is effective in ensuring the bone heals correctly.
- Surgical Intervention: In cases where the bone is misaligned, displaced, or involves complex fractures, surgery may be necessary to realign the bones and secure them with hardware such as plates, screws, or rods.
- Rehabilitation: Once the bone begins healing, physical therapy and rehabilitation are often recommended to restore function, strength, and mobility.
The Importance of Proper Fracture Care
Proper fracture care is essential to ensure a smooth recovery and prevent long-term complications. This includes ensuring the bone heals in the correct position, minimizing the risk of infection (in cases where surgery is required), and supporting the joint or limb through rehabilitation.
Fracture management is tailored to each individual’s needs, taking into consideration the type and location of the fracture, as well as the patient’s overall health and activity level. Timely and appropriate treatment plays a vital role in helping patients return to their normal activities as quickly and safely as possible.
Interventional Radiology
Interventional Radiology
Interventional radiology (IR) offers minimally invasive, image-guided injections to manage pain and inflammation in various parts of the body. These procedures provide targeted relief for conditions such as arthritis, bursitis, and chronic pain syndromes.
Common Types of Injections in Interventional Radiology
- Joint Injections
Joint injections help manage pain and inflammation caused by arthritis, injuries, or degenerative conditions. Medications such as corticosteroids, hyaluronic acid, or platelet-rich plasma (PRP) are administered under image guidance to ensure precise delivery.
- Soft Tissue Injections
Soft tissue injections target areas such as tendons, ligaments, and bursae to reduce inflammation and promote healing. These are commonly used for conditions like tendonitis and bursitis.
- Nerve Blocks
Nerve block injections involve the administration of anesthetics or anti-inflammatory medications near nerves to interrupt pain signals. These injections can be used for chronic pain management and diagnostic purposes.
- Epidural Injections
Epidural injections deliver anti-inflammatory medication into the space around the spinal cord to relieve pain from conditions such as herniated discs and spinal stenosis.
Benefits of Image-Guided Injections
- Precision: Fluoroscopy or ultrasound ensures accurate needle placement.
- Minimally Invasive: Quick procedure with minimal recovery time.
- Effective Pain Relief: Reduces inflammation and enhances mobility.
- Outpatient Procedure: No hospital stay required.
Risks and Considerations
While generally safe, potential risks include:
- Temporary soreness at the injection site
- Rare risk of infection
- Temporary numbness or weakness
Conclusion
Interventional radiology injections provide an effective, non-surgical option for pain relief in joints, soft tissues, and nerves. If chronic pain affects your daily life, consult an interventional radiologist to explore targeted treatment options.
Robotic Assisted Total Hip Arthroplasty
Robotic Assisted Total Hip Arthroplasty
Robotic-assisted total hip arthroplasty (THA) using the MAKO system is an advanced, minimally invasive procedure designed to enhance the precision and outcomes of hip replacement surgery. Combined with the direct anterior approach (DAA), this technique allows orthopedic surgeons to perform hip replacement with greater accuracy, preserving soft tissue and enabling a faster recovery.
What Is Robotic-Assisted Hip Surgery with the MAKO System?
The MAKO robotic system utilizes 3D imaging and real-time data to assist the surgeon in performing the hip replacement with unmatched precision. A pre-operative CT scan creates a detailed map of the patient’s hip joint, allowing for a personalized surgical plan. During the procedure, the robotic arm helps the surgeon make precise bone cuts and implant adjustments, ensuring optimal alignment and fit—critical factors for joint function and implant longevity.
When Is Robotic-Assisted Hip Surgery Used?
The MAKO system is typically recommended for patients with:
- Severe Osteoarthritis: Individuals suffering from chronic hip pain, stiffness, and reduced mobility due to cartilage degeneration.
- Hip Joint Damage: Patients with significant hip joint deterioration from injury, trauma, or wear overtime.
- Deformities or Misalignment: Those with structural abnormalities affecting joint stability and movement.
Benefits of Robotic-Assisted Hip Surgery with the MAKO System and Direct Anterior Approach
- Enhanced Precision: Robotic assistance ensures accurate implant positioning, leading to better function and longevity.
- Minimally Invasive: The direct anterior approach involves smaller incisions, preserving surrounding muscles and soft tissues.
- Faster Recovery: Patients often experience reduced pain, a shorter hospital stay, and quicker return to daily activities.
- Improved Stability: The anterior approach lowers the risk of dislocation compared to traditional methods.
- Personalized Surgery: 3D pre-surgical planning allows for a customized implant fit, improving long-term outcomes.
For those suffering from hip pain and considering total hip replacement, robotic-assisted THA with the MAKO system and the direct anterior approach offers an innovative, precise, and minimally invasive solution. This advanced approach enhances surgical accuracy, recovery speed, and long-term implant performance.
Carpal Tunnel Release Surgery
Carpal Tunnel Release Surgery: Overview, Indications, and Recovery
Carpal tunnel release surgery is a common procedure used to treat carpal tunnel syndrome, a condition that results from pressure on the median nerve as it passes through the carpal tunnel in the wrist. During the surgery, the ligament pressing on the nerve is cut to relieve pressure and alleviate symptoms like pain, numbness, and weakness in the hand.
Indications for Carpal Tunnel Release Surgery
Carpal tunnel release surgery may be recommended for patients experiencing persistent symptoms of carpal tunnel syndrome that do not improve with conservative treatments. Conditions that may indicate the need for surgery include:
- Severe Carpal Tunnel Syndrome: When symptoms like numbness, tingling, or pain in the hand and wrist become severe and affect daily activities.
- Chronic Numbness or Weakness: If there is significant weakness in the hand or the inability to perform tasks due to loss of sensation or strength.
- Failed Conservative Treatments: When non-surgical options like wrist splints, physical therapy, or corticosteroid injections do not provide relief.
- Atrophy of Hand Muscles: In advanced cases, when the muscles at the base of the thumb begin to shrink due to nerve damage from prolonged pressure.
Procedure for Carpal Tunnel Release Surgery
Carpal tunnel release surgery is usually performed on an outpatient basis under local anesthesia, though some patients may require general anesthesia depending on their preferences and the complexity of the procedure. The steps involved include:
- Incision: A small incision is made in the palm of the hand or wrist, over the carpal tunnel.
- Release of the Ligament: The surgeon cuts the transverse carpal ligament, which forms the roof of the carpal tunnel, to relieve the pressure on the median nerve.
- Closing: The incision is closed with stitches or adhesive strips, and a bandage is applied to the area.
Benefits of Carpal Tunnel Release Surgery
- Effective Relief from Symptoms: Carpal tunnel release surgery is highly effective in relieving the numbness, tingling, and pain caused by carpal tunnel syndrome.
- Minimally Invasive: The procedure is typically performed with minimal disruption to surrounding tissues, leading to less pain and a faster recovery compared to more invasive surgeries.
- Improved Hand Function: Many patients experience significant improvements in hand strength, dexterity, and the ability to perform daily activities after recovery.
- Long-Term Solution: The surgery provides a long-term solution for carpal tunnel syndrome, with a low recurrence rate of symptoms.
Symptoms or Conditions Treated by Carpal Tunnel Release Surgery
Carpal tunnel release surgery is intended to treat the following symptoms and conditions related to carpal tunnel syndrome:
- Numbness or Tingling: Persistent numbness or tingling in the thumb, index, middle, or ring fingers, particularly at night or after repetitive hand movements.
- Pain: Ongoing pain in the wrist, hand, or fingers that may radiate up the arm.
- Weakness: Weakness in the hand, leading to difficulty gripping or performing tasks that require fine motor skills.
- Atrophy: In advanced stages, muscle wasting at the base of the thumb (thenar atrophy) may occur.
Recovery and Rehabilitation After Carpal Tunnel Release Surgery
Recovery from carpal tunnel release surgery generally involves a few key stages:
- Initial Recovery:
- Rest and Immobilization: A bandage or splint is typically worn for several days to protect the wrist and limit movement while it heals.
- Pain Management: Over-the-counter pain relievers (e.g., ibuprofen) or prescribed medication can help manage discomfort during the recovery phase.
- Physical Therapy:
- Wrist Exercises: Once the initial healing has occurred, gentle range-of-motion exercises may be introduced to restore flexibility and strength to the wrist and hand.
- Strengthening Exercises: After a few weeks, strengthening exercises may help improve grip strength and overall function of the hand.
- Return to Activity:
- Most patients can return to light activities within a few weeks, but more strenuous activities may require 4-6 weeks for full recovery.
- Full recovery typically takes 2-3 months, with gradual improvement in hand function over this period.
Risks of Carpal Tunnel Release Surgery
While carpal tunnel release surgery is generally safe, there are some risks to be aware of, including:
- Infection: As with any surgery, there is a risk of infection at the incision site.
- Nerve Injury: Although rare, there is a slight risk of injury to the median nerve or surrounding structures during the procedure.
- Scar Tissue: Some patients may develop scar tissue at the site of the incision, which could cause stiffness or discomfort.
- Incomplete Symptom Relief: In some cases, surgery may not fully resolve symptoms, especially if there is nerve damage that has progressed over time.
- Post-Surgical Pain: Mild pain or swelling may persist for a few weeks after surgery as the wrist heals.
Carpal tunnel release surgery is an effective treatment option for relieving the symptoms of carpal tunnel syndrome and improving hand function. While the recovery process typically involves some rehabilitation, the long-term benefits of symptom relief and improved quality of life are significant. If you are considering carpal tunnel release surgery, consult with your healthcare provider to discuss whether it is the right treatment option for you.
Trigger Finger Release Surgery
Trigger Finger Release Surgery: Overview, Indications, and Recovery
Trigger finger release surgery is a common procedure used to treat a condition called trigger finger (also known as stenosing tenosynovitis), which causes the fingers to catch or lock in a bent position. The surgery involves cutting a ligament in the hand to relieve pressure on the tendon, allowing the finger to move freely again.
Indications for Trigger Finger Release Surgery
Trigger finger release surgery is typically recommended when conservative treatments, such as rest, splints, or steroid injections, fail to relieve symptoms. Surgery is often considered for:
- Persistent Locking or Catching: When the finger repeatedly gets stuck in a bent position and can only be straightened with force.
- Pain: Chronic pain or tenderness in the affected finger, especially during activities that involve gripping or making a fist.
- Limited Finger Movement: Difficulty straightening the finger, even after conservative treatments.
- Failure of Non-Surgical Treatments: When other options, such as anti-inflammatory medications, physical therapy, or injections, do not improve symptoms.
Procedure for Trigger Finger Release Surgery
Trigger finger release surgery is generally performed as an outpatient procedure under local anesthesia. The steps involved include:
- Incision: A small incision is made in the palm or the base of the affected finger.
- Release of the A1 Pulley: The surgeon cuts the A1 pulley, a ligament that is pressing on the tendon, causing the finger to get stuck. This release allows the tendon to move freely again.
- Closing: After the ligament is released, the incision is closed with stitches or adhesive strips. The hand is bandaged to reduce swelling and protect the surgical site.
Benefits of Trigger Finger Release Surgery
- Effective Symptom Relief: The surgery provides relief from the pain, locking, and catching associated with trigger finger.
- Improved Finger Mobility: Once the surgery site heals, patients often regain full or nearly full range of motion in the affected finger.
- Minimally Invasive: The procedure is typically done through a small incision, leading to a faster recovery and minimal scarring.
- Long-Term Solution: Trigger finger release surgery offers a long-lasting solution, with a low recurrence rate of symptoms after recovery.
Symptoms or Conditions Treated by Trigger Finger Release Surgery
Trigger finger release surgery is specifically used to treat the following symptoms and conditions associated with trigger finger:
- Finger Locking or Catching: The finger becomes stuck in a bent position and may need to be manually straightened.
- Pain: Persistent pain in the finger, especially when trying to bend or straighten it.
- Swelling: Swelling at the base of the finger or at the joint where the tendon is catching.
- Difficulty Moving the Finger: Reduced range of motion in the affected finger, particularly when making a fist or gripping objects.
Recovery and Rehabilitation After Trigger Finger Release Surgery
Recovery from trigger finger release surgery generally follows a structured process:
- Initial Recovery:
- Rest and Immobilization: A splint may be used for a few days to immobilize the finger and reduce movement during the initial healing phase.
- Pain Management: Over-the-counter pain relievers (e.g., ibuprofen) or prescribed medication can help manage any post-surgical discomfort.
- Physical Therapy:
- Gentle Exercises: After a few days or weeks, range-of-motion exercises may be introduced to help restore flexibility and movement in the finger.
- Strengthening: Once healing progresses, strengthening exercises can be started to improve grip strength and finger mobility.
- Return to Activity:
- Most patients can resume light activities within a week or two after surgery, but more strenuous tasks may take 4–6 weeks for full recovery.
- Full recovery is usually achieved within 1–2 months, with gradual improvement in finger movement and function.
Risks of Trigger Finger Release Surgery
Though trigger finger release surgery is generally safe, there are some risks to be aware of:
- Infection: As with any surgical procedure, there is a small risk of infection at the incision site.
- Nerve Injury: There is a rare risk of injury to nearby nerves, which could cause numbness or weakness in the finger.
- Scar Tissue: In some cases, scar tissue may develop around the tendon, potentially limiting movement or causing discomfort.
- Stiffness: Some patients may experience stiffness in the finger after surgery, although this typically resolves with rehabilitation.
- Recurrence of Symptoms: While uncommon, trigger finger symptoms can return after surgery, especially if the underlying cause of the condition is not addressed.
Trigger finger release surgery is a highly effective treatment for resolving the pain, locking, and restricted movement caused by trigger finger. With a quick recovery and minimal risk of recurrence, it provides a long-term solution for many patients. If you’re considering surgery for trigger finger, consult with a healthcare professional to determine if it’s the right option for you.
First Dorsal Compartment Release Surgery
First Dorsal Compartment Release Surgery: Overview, Indications, and Recovery
First dorsal compartment release surgery is commonly used to treat a condition known as De Quervain’s tenosynovitis, which causes pain and swelling along the thumb side of the wrist. This condition occurs when the tendons that control thumb movement become irritated or inflamed due to excessive use or injury. The surgery involves releasing the sheath surrounding these tendons to relieve pressure and reduce inflammation.
Indications for First Dorsal Compartment Release Surgery
First dorsal compartment release surgery is typically recommended when conservative treatments, such as splinting, nonsteroidal anti-inflammatory drugs (NSAIDs), or corticosteroid injections, do not provide sufficient relief. It may be considered for:
- Persistent Pain: Chronic pain along the thumb side of the wrist that does not improve with rest or medication.
- Swelling and Tenderness: Swelling or tenderness over the first dorsal compartment, especially when gripping, twisting, or making a fist.
- Reduced Thumb Function: Difficulty using the thumb for daily activities, such as holding objects or turning keys, due to pain or limited movement.
- Failed Non-Surgical Treatments: When other treatments, including therapy or injections, fail to relieve symptoms.
Procedure for First Dorsal Compartment Release Surgery
First dorsal compartment release surgery is typically performed on an outpatient basis under local anesthesia, though some patients may require regional or general anesthesia. The steps involved include:
- Incision: A small incision is made on the side of the wrist near the base of the thumb, over the first dorsal compartment.
- Release of Tendon Sheath: The surgeon cuts the ligament that forms the roof of the first dorsal compartment, which surrounds the tendons of the thumb. This release reduces pressure on the tendons and alleviates pain.
- Closing: After the release is performed, the incision is closed with stitches or adhesive strips, and a bandage is applied to protect the area.
Benefits of First Dorsal Compartment Release Surgery
- Effective Pain Relief: The surgery offers significant relief from the pain, swelling, and discomfort associated with De Quervain’s tenosynovitis.
- Improved Thumb Function: Once healed, most patients regain full or nearly full thumb mobility, improving their ability to perform daily tasks.
- Minimally Invasive: The procedure is typically performed through a small incision, which reduces scarring and the risk of complications.
- Long-Term Solution: First dorsal compartment release surgery provides a long-lasting solution for those who have not responded to other treatments, with a low recurrence rate of symptoms.
Symptoms or Conditions Treated by First Dorsal Compartment Release Surgery
First dorsal compartment release surgery is specifically designed to treat the following symptoms and conditions related to De Quervain’s tenosynovitis:
- Pain at the Base of the Thumb: Pain, especially when gripping or rotating the wrist, is a hallmark symptom of De Quervain’s tenosynovitis.
- Swelling: Swelling along the thumb side of the wrist, particularly around the first dorsal compartment.
- Tenderness: Pain or tenderness when pressing on the area over the tendons that control thumb movement.
- Difficulty with Thumb Movement: Limited ability to move the thumb, especially when performing tasks that require grasping or twisting.
Recovery and Rehabilitation After First Dorsal Compartment Release Surgery
Recovery from first dorsal compartment release surgery typically follows a structured process:
- Initial Recovery:
- Rest and Immobilization: A splint or brace may be used to protect the wrist and limit movement during the early healing phase.
- Pain Management: Over-the-counter pain relievers (e.g., ibuprofen) or prescribed medications can help manage post-surgical discomfort.
- Physical Therapy:
- Gentle Exercises: After a few days or weeks, rehabilitation exercises may be introduced to improve the range of motion and flexibility of the wrist and thumb.
- Strengthening: Once healing progresses, strengthening exercises can help restore function and prevent stiffness.
- Return to Activity:
- Most patients can return to light activities within 2–3 weeks after surgery, though more strenuous tasks may take 4–6 weeks.
- Full recovery typically takes 2–3 months, with gradual improvement in thumb and wrist function.
Risks of First Dorsal Compartment Release Surgery
Although first dorsal compartment release surgery is generally safe, there are some potential risks to consider:
- Infection: As with any surgery, there is a small risk of infection at the incision site.
- Nerve Injury: There is a rare risk of injury to nearby nerves, which could cause numbness or weakness in the hand or wrist.
- Scar Tissue: Some patients may develop scar tissue around the tendons or incision site, potentially leading to stiffness or discomfort.
- Failure to Relieve Symptoms: In some cases, symptoms may persist after surgery, requiring additional treatment.
- Stiffness or Reduced Range of Motion: Some patients may experience temporary stiffness or reduced motion in the wrist or thumb, although this typically improves with physical therapy.
First dorsal compartment release surgery is an effective solution for treating De Quervain’s tenosynovitis and providing long-term relief from thumb and wrist pain. The procedure is minimally invasive and offers significant benefits in terms of pain reduction and restored function. If conservative treatments have not provided sufficient relief, consult with a healthcare provider to determine if this surgery is the right option for you.
CMC Arthroplasty Surgery
CMC Arthroplasty Surgery: Overview, Indications, and Recovery
CMC (carpometacarpal) arthroplasty is a surgical procedure used to treat pain and dysfunction in the thumb joint, particularly at the base of the thumb where the first metacarpal meets the trapezium bone (CMC joint). The procedure involves removing or replacing the damaged joint with a prosthetic or reconstructing it to restore function and alleviate pain, often due to arthritis or other degenerative conditions.
Indications for CMC Arthroplasty Surgery
CMC arthroplasty is typically considered for individuals experiencing chronic pain, limited motion, and reduced hand function due to various conditions affecting the CMC joint, including:
- Osteoarthritis: Degenerative joint disease that causes pain, stiffness, and reduced range of motion in the thumb, particularly at the base.
- Rheumatoid Arthritis: An autoimmune disorder that leads to inflammation and deformity in the CMC joint.
- Post-Traumatic Arthritis: Joint degeneration following a fracture or injury to the thumb.
- Failed Conservative Treatments: When non-surgical options, such as splinting, medications, or injections, do not provide sufficient relief.
- Severe Thumb Deformity: When arthritis or injury causes significant changes to the thumb’s alignment and function.
Procedure for CMC Arthroplasty Surgery
CMC arthroplasty is usually performed under local anesthesia, with or without sedation, and involves the following steps:
- Incision: A small incision is made at the base of the thumb over the CMC joint.
- Joint Removal or Reconstruction: The damaged portion of the CMC joint may be removed, and in some cases, a prosthetic implant is used to replace the joint. Alternatively, the surgeon may reconstruct the joint by using a tendon from the patient’s own body to stabilize the joint.
- Closing: After the procedure, the incision is closed with sutures or adhesive strips, and a bandage is applied to the surgical site.
Benefits of CMC Arthroplasty Surgery
- Pain Relief: The procedure provides significant pain relief, allowing patients to resume daily activities without discomfort.
- Improved Function and Mobility: CMC arthroplasty helps restore thumb movement, which is crucial for gripping and pinching tasks.
- Long-Term Solution: The surgery provides a durable, long-lasting solution for thumb arthritis, with many patients experiencing relief for years.
- Minimally Invasive Options: Some techniques, like the use of small incisions and minimal disruption of surrounding tissues, lead to quicker recovery and less scarring.
Symptoms or Conditions Treated by CMC Arthroplasty Surgery
CMC arthroplasty is primarily used to treat conditions affecting the thumb joint, including:
- Severe Pain: Chronic pain in the base of the thumb, especially with gripping, pinching, or turning objects.
- Limited Range of Motion: Difficulty in moving the thumb, especially when performing tasks that involve grasping or lifting.
- Thumb Weakness: Weakness in the thumb, which can limit the ability to hold or manipulate objects.
- Deformity: Changes in thumb alignment or joint deformity caused by arthritis or injury.
Recovery and Rehabilitation After CMC Arthroplasty Surgery
Recovery from CMC arthroplasty surgery typically involves the following stages:
- Initial Recovery:
- Rest and Immobilization: A splint or cast may be used to immobilize the thumb and wrist during the initial recovery period, typically for 2-4 weeks.
- Pain Management: Pain can be managed with medications such as NSAIDs or prescribed pain relievers, as well as ice therapy to reduce swelling.
- Physical Therapy:
- Range of Motion Exercises: After the initial healing phase, rehabilitation exercises are introduced to restore thumb and hand movement.
- Strengthening Exercises: Gradual strengthening exercises help rebuild strength and prevent stiffness in the thumb and wrist.
- Return to Activity:
- Most patients can return to light activities within 4-6 weeks, but more demanding tasks may take 3-6 months depending on the type of surgery and the patient’s progress.
- Full recovery is typically achieved within 3-6 months, with continued improvement in thumb function as rehabilitation progresses.
Risks of CMC Arthroplasty Surgery
While CMC arthroplasty is generally safe, there are potential risks to consider, including:
- Infection: As with any surgical procedure, there is a risk of infection at the incision site or within the joint.
- Nerve Injury: Rarely, nearby nerves may be injured during surgery, leading to numbness, tingling, or weakness in the thumb.
- Implant Failure: If a prosthetic implant is used, it may wear out or loosen over time, requiring additional surgery or revision.
- Stiffness: Some patients may experience temporary stiffness in the thumb or wrist, although this can often be improved with physical therapy.
- Blood Clots: As with any surgery, there is a small risk of developing blood clots, especially in the lower legs.
CMC arthroplasty surgery is an effective treatment option for individuals with chronic pain and dysfunction due to arthritis or injury in the thumb. By restoring joint function and alleviating pain, the procedure significantly improves quality of life and allows for a return to daily activities. If you are considering this surgery, consult with your healthcare provider to determine whether it is the right option for your condition.
Excision of Hand & Wrist Cysts
Excision of Hand and Wrist Cysts: Overview, Indications, and Recovery
An excision biopsy is a surgical procedure used to remove cysts or abnormal growths from the hand or wrist for diagnostic or therapeutic purposes. The procedure involves the complete removal of the cyst along with a portion of surrounding tissue, which is then sent to a lab for pathological examination. This allows for both treatment of the cyst and an accurate diagnosis to rule out any underlying conditions, including infections, tumors, or other abnormalities.
Indications for Excision Biopsy of Hand and Wrist Cysts
Excision biopsy is recommended when a cyst or mass in the hand or wrist is causing symptoms such as pain, discomfort, or functional limitations. It is also indicated when the cyst’s nature is unclear, and further diagnostic investigation is needed. Common indications include:
- Persistent or Painful Cysts: When a cyst causes chronic pain, discomfort, or limits the movement of the hand or wrist.
- Increased Size: A cyst that continues to grow or changes in appearance over time may require removal to prevent complications.
- Suspected Tumors or Malignancy: If there is concern that the cyst may be cancerous or have malignant characteristics, an excision biopsy is essential for diagnosis.
- Infection or Abscess: In cases where the cyst is infected or causing an abscess, excision can help eliminate the source of the infection.
- Functional Limitations: When a cyst interferes with the ability to perform daily tasks or use the hand or wrist, removal may be necessary to restore function.
Procedure for Excision Biopsy of Hand and Wrist Cysts
Excision biopsy of hand and wrist cysts is typically performed as an outpatient procedure, with local anesthesia to numb the area. The steps of the procedure include:
- Anesthesia: Local anesthesia is administered to numb the area around the cyst, ensuring that the patient is comfortable during the procedure.
- Incision: A small incision is made directly over the cyst or mass, allowing the surgeon to access and remove the cyst and surrounding tissue.
- Cyst Removal: The entire cyst is carefully excised, along with any adjacent tissue that may be necessary for an accurate diagnosis. The cyst may be a ganglion cyst, epidermoid cyst, or another type of growth.
- Examination: The removed tissue is sent to a laboratory for pathological analysis to determine its nature and whether it is benign or malignant.
- Closing: The incision is closed using sutures, and a sterile bandage is applied to the surgical site.
Benefits of Excision Biopsy of Hand and Wrist Cysts
- Diagnosis and Treatment in One Procedure: Excision biopsy allows for both the removal of the cyst and the collection of tissue for diagnostic evaluation, providing a clear diagnosis.
- Pain and Symptom Relief: By removing the cyst, the procedure alleviates associated pain, swelling, or functional impairments in the hand or wrist.
- Prevention of Recurrence: Complete removal of the cyst reduces the likelihood of it returning in the future.
- Minimally Invasive: The procedure is generally performed with small incisions, minimizing scarring and reducing recovery time.
Symptoms or Conditions Treated by Excision Biopsy of Hand and Wrist Cysts
Excision biopsy is primarily used to treat cysts or masses in the hand or wrist, including:
- Ganglion Cysts: Fluid-filled lumps that often develop along tendons or joints in the wrist or hand.
- Epidermoid Cysts: Benign cysts that form under the skin, often filled with keratin or dead skin cells.
- Lipomas: Benign fatty tumors that can form in the soft tissues of the hand or wrist.
- Other Soft Tissue Cysts or Masses: Various types of cysts or tumors that can develop in the soft tissues of the hand or wrist.
Recovery and Rehabilitation After Excision Biopsy of Hand and Wrist Cysts
The recovery process after an excision biopsy depends on the size and location of the cyst, but generally involves the following stages:
- Initial Recovery:
- Rest and Elevation: The hand or wrist may need to be rested and elevated during the first few days to minimize swelling.
- Pain Management: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, are typically recommended to manage pain and inflammation.
- Wound Care: The incision site will need to be kept clean and dry, with any sutures being removed in about 7–10 days.
- Physical Therapy (if necessary):
- Gentle Exercises: Once healing begins, some patients may be advised to perform gentle stretching exercises to prevent stiffness in the hand or wrist.
- Strengthening: If the cyst was located in an area that affected movement, strengthening exercises may be incorporated into rehabilitation after the initial healing phase.
- Return to Activity:
- Most patients can return to normal activities within 1–2 weeks, depending on the location and extent of the excision. Strenuous activities, such as heavy lifting or sports, should generally be avoided for 4–6 weeks.
- Full recovery can take several weeks, with the final result depending on the size of the cyst and the extent of the incision.
Risks of Excision Biopsy of Hand and Wrist Cysts
While excision biopsy is generally a safe procedure, there are potential risks to consider:
- Infection: There is always a risk of infection at the incision site.
- Nerve Injury: In rare cases, nerves near the cyst may be injured during the procedure, leading to numbness or weakness in the hand or wrist.
- Scarring: Though the incisions are small, some scarring may occur, particularly if the cyst is large or the incision is extensive.
- Recurrence: While excision reduces the chances of recurrence, some cysts may return, especially if they were not fully removed.
- Bleeding: Some bleeding may occur during the procedure, but this is typically minimal.
Excision biopsy of hand and wrist cysts offers an effective solution for both diagnosing and treating cysts that cause pain, discomfort, or dysfunction. By completely removing the cyst and obtaining tissue for analysis, this procedure provides clarity on the nature of the growth and offers significant relief for patients. If you have a cyst in the hand or wrist that is causing symptoms or concern, consult with your healthcare provider to determine whether excision biopsy is the right treatment for you.
Thumb Ulnar Collateral Ligament Reconstruction
Thumb Ulnar Collateral Ligament (UCL) Injury Reconstruction Surgery: Overview, Indications, and Recovery
Thumb ulnar collateral ligament (UCL) injury reconstruction surgery is a procedure performed to repair or reconstruct the UCL ligament at the base of the thumb, typically caused by trauma, hyperextension, or overuse. The UCL plays a crucial role in stabilizing the thumb joint, especially during gripping and pinching motions. A UCL tear can result in pain, instability, and loss of thumb function, making this surgery a vital option for restoring stability and motion in the thumb.
What is a Thumb Ulnar Collateral Ligament (UCL) Injury?
The ulnar collateral ligament (UCL) is a key ligament that connects the thumb’s metacarpal bone to the proximal phalanx, providing stability to the thumb joint. When the UCL is torn or ruptured, often due to trauma, such as a forced bend or hyperextension (e.g., a fall or sports-related injury), the thumb can become unstable. This instability can make it difficult to perform everyday tasks that require grip or pinching, such as opening jars, writing, or playing sports.
In some cases, especially when the injury is severe or chronic, non-surgical treatments like rest, splinting, and physical therapy may not be enough. Thumb UCL injury reconstruction surgery becomes necessary to restore the ligament’s function and stabilize the thumb.
Indications for Thumb Ulnar Collateral Ligament Injury Reconstruction Surgery
Thumb UCL injury reconstruction surgery is typically considered when conservative treatments fail to provide relief or if the ligament is significantly torn. Some of the main indications for surgery include:
- Severe UCL Tear: Complete or substantial tearing of the UCL, which cannot heal with rest or splinting.
- Instability: Persistent thumb instability, resulting in difficulty gripping, pinching, or performing tasks requiring fine motor control.
- Chronic Pain: Ongoing pain at the base of the thumb that doesn’t improve with rest, splinting, or medications.
- Loss of Function: Difficulty performing daily activities due to decreased thumb function caused by ligament damage.
- Failure of Non-Surgical Treatments: Conservative treatments like rest, physical therapy, or injections haven’t provided sufficient improvement.
Procedure for Thumb Ulnar Collateral Ligament (UCL) Injury Reconstruction Surgery
The surgery to reconstruct or repair the UCL ligament typically involves several key steps:
- Anesthesia: Thumb UCL injury reconstruction surgery is usually performed under local anesthesia with a regional nerve block, ensuring that the thumb and hand are numb during the procedure. In more complex cases, general anesthesia may be used.
- Incision: A small incision is made at the base of the thumb, near the site of the UCL. This allows the surgeon to access the ligament and surrounding structures.
- UCL Repair or Reconstruction
- Repair: If the ligament is torn but can be reattached, the surgeon will use sutures to reconnect the torn ends of the ligament.
- Reconstruction: If the ligament is extensively damaged, the surgeon may reconstruct the UCL using a tendon graft (often taken from the forearm or other areas of the body). The tendon is used to replace the damaged ligament, allowing the thumb joint to regain stability.
- Tensioning the Ligament: The surgeon ensures that the ligament or tendon graft is appropriately tensioned to restore thumb stability, making sure that it will hold under normal functional loads.
- Closing the Incision: After the repair or reconstruction is complete, the surgeon closes the incision with sutures. A bandage or splint is applied to the thumb to protect it during the healing phase.
Benefits of Thumb Ulnar Collateral Ligament Injury Reconstruction Surgery
- Restored Stability: The surgery helps restore the stability of the thumb joint, allowing for normal thumb movement and grip function.
- Pain Relief: Alleviates chronic pain at the base of the thumb, improving comfort during activities.
- Improved Function: With the ligament repaired or reconstructed, the thumb regains its ability to grip, pinch, and perform other important tasks.
- Prevention of Long-Term Disability: Proper surgical intervention can prevent long-term disability or deformity that could result from an untreated UCL injury.
Recovery and Rehabilitation After Thumb Ulnar Collateral Ligament (UCL) Injury Reconstruction Surgery
Recovery after thumb UCL injury reconstruction surgery typically involves several stages, including initial immobilization, rehabilitation, and gradual return to activity.
- Initial Recovery
- Immobilization: After surgery, the thumb is usually immobilized with a splint or cast for 4–6 weeks to allow the ligament to heal and protect the surgical site.
- Pain Management: Pain is typically managed with prescribed medications (e.g., NSAIDs) and ice therapy to reduce swelling and discomfort.
- Physical Therapy
- Early Rehabilitation: Once the initial healing period has passed, patients begin physical therapy to regain range of motion and reduce stiffness in the thumb.
- Strengthening: As healing progresses, strengthening exercises are introduced to rebuild the muscles around the thumb and hand.
- Gradual Return to Activities: Most patients can resume light activities after 8–12 weeks, with full return to more strenuous activities, such as sports or heavy lifting, taking 3–6 months.
- Long-Term Care
- Full recovery from UCL reconstruction surgery typically takes 3 to 6 months, depending on the severity of the injury and the individual’s healing process.
- Ongoing physical therapy may be necessary to optimize thumb strength, flexibility, and function after the surgery.
Risks of Thumb Ulnar Collateral Ligament Injury Reconstruction Surgery
While thumb UCL injury reconstruction surgery is generally safe, there are potential risks, including:
- Infection: As with any surgical procedure, there is a risk of infection at the surgical site.
- Nerve Injury: Rarely, nearby nerves may be damaged during surgery, leading to numbness, tingling, or weakness.
- Stiffness: Some patients may develop stiffness in the thumb joint or surrounding tissues, limiting motion.
- Recurrence of Instability: In rare cases, the repaired or reconstructed ligament may tear again, especially if the thumb is subjected to high-stress activities before healing is complete.
- Failure to Restore Full Function: The surgery may not fully restore thumb stability or functionality in some cases, requiring further treatment or surgical intervention.
Conclusion
Thumb ulnar collateral ligament (UCL) injury reconstruction surgery is an effective option for treating severe UCL tears, instability, and chronic pain at the base of the thumb. By repairing or reconstructing the ligament, this surgery helps restore normal thumb function, allowing for improved stability, grip strength, and overall thumb movement. If you are experiencing thumb instability, pain, or difficulty performing daily tasks due to a UCL injury, consult with an orthopedic or hand surgeon to determine if this surgery is the right solution for your condition. Proper rehabilitation and adherence to recovery guidelines are essential for achieving the best possible outcome.
Arthrodesis
Arthrodesis of the Hand and Wrist: Overview, Indications, and Recovery
Arthritis surgery fusion, also known as arthrodesis, is a surgical procedure used to treat arthritis in the hand and wrist by permanently fusing the bones of a joint. This procedure aims to relieve pain, improve function, and stabilize the affected joint, particularly when arthritis has led to severe degeneration and there is little to no cartilage left for proper joint movement. Fusion surgery is often recommended when non-surgical treatments, such as medications or physical therapy, have failed to provide relief.
What is Arthritis Surgery Fusion (Arthrodesis)?
Arthritis in the hand and wrist occurs when the cartilage that cushions the bones within the joints breaks down, leading to pain, swelling, and reduced mobility. In advanced cases of arthritis, when the joint surfaces are severely damaged, fusion surgery may be considered. The goal of the surgery is to remove the damaged cartilage and fuse the bones together, so they heal as one solid unit. This fusion eliminates the pain caused by arthritis but also reduces joint movement.
Arthritis surgery fusion can be performed on various joints in the hand and wrist, such as the wrist joint, the base of the thumb (CMC joint), or finger joints, depending on the location of the arthritis.
Indications for Arthritis Surgery Fusion for Hand and Wrist
Arthritis surgery fusion may be recommended in the following situations:
- Severe Arthritis: When arthritis has caused significant damage to the joint, and other non-surgical treatments have failed.
- Chronic Pain: When pain from arthritis is constant and debilitating, interfering with daily activities.
- Limited Mobility: When joint movement is severely restricted, making it difficult to perform everyday tasks.
- Instability: In cases where arthritis has led to joint instability, fusion can help stabilize the joint.
- Failure of Conservative Treatments: When other treatment options, such as medication, injections, or splints, are no longer effective.
- End-Stage Arthritis: When there is little or no cartilage left in the joint and movement is limited or painful.
Procedure for Arthritis Surgery Fusion (Arthrodesis) for Hand and Wrist
Arthritis surgery fusion is typically performed under local anesthesia with sedation or general anesthesia, depending on the complexity and the joint involved. The procedure involves several steps:
- Anesthesia: The patient will either receive local anesthesia (with or without sedation) or general anesthesia, depending on the complexity of the surgery and the joint involved.
- Incision: The surgeon makes an incision over the affected joint to expose the bones that need to be fused. The incision size will depend on the joint being treated.
- Joint Preparation: The damaged cartilage and any arthritic tissue are removed from the joint surfaces to prepare the bones for fusion. The surgeon will then carefully align the bones of the joint in the correct position.
- Bone Fusion: The bones are then held together using hardware, such as screws, plates, or pins, to maintain proper alignment while they fuse. In some cases, bone graft material may be used to encourage the fusion process.
- Closing the Incision: After the bones are securely fused, the surgeon will close the incision with sutures. A bandage or splint will be applied to support the hand or wrist while it heals.
Benefits of Arthritis Surgery Fusion for Hand and Wrist
- Pain Relief: Fusion surgery can eliminate the pain associated with arthritis, especially when conservative treatments no longer provide relief.
- Joint Stability: The procedure stabilizes the joint, reducing the risk of further damage or deformity.
- Improved Function: While the procedure limits joint movement, it can still provide improved function in many cases, allowing patients to perform necessary tasks without pain.
- Long-Term Solution: Arthrodesis provides a durable, long-term solution for joint degeneration, especially in patients with end-stage arthritis.
- Reduced Risk of Deformity: By stabilizing the joint, fusion surgery can prevent further deformity or malalignment of the hand or wrist joint.
Recovery and Rehabilitation After Arthritis Surgery Fusion
Recovery after arthritis surgery fusion typically involves a period of immobilization, followed by rehabilitation. Here’s what you can expect:
- Initial Recovery
- Immobilization: After surgery, the hand or wrist will be immobilized in a cast or splint for several weeks to allow the bones to heal and fuse together.
- Pain Management: Pain is generally managed with medications, including NSAIDs or stronger pain relievers, as needed. Ice packs can help reduce swelling and discomfort.
- Elevation: Keeping the hand elevated during the initial healing phase can help minimize swelling.
- Physical Therapy
- Early Rehabilitation: Once the bones have fused and the initial healing period has passed (usually around 6–8 weeks), physical therapy will begin. Therapy focuses on restoring strength, mobility, and function in the hand or wrist.
- Range of Motion: Exercises will be introduced gradually to maintain or improve flexibility and movement in other joints of the hand or wrist.
- Strengthening: As healing progresses, strengthening exercises are introduced to rebuild the muscles surrounding the fused joint.
- Long-Term Care
- Fusion Process: It may take several months (typically 3–6 months) for the bones to fully fuse. During this time, the hand or wrist may be kept in a brace or splint to prevent movement.
- Gradual Return to Activity: Once the fusion has fully occurred and strength has been regained, most patients can return to normal activities. However, certain activities that place stress on the fused joint may need to be limited.
Risks of Arthritis Surgery Fusion for Hand and Wrist
As with any surgery, arthritis surgery fusion carries some risks, including:
- Infection: There is always a risk of infection at the incision site or within the joint.
- Nonunion or Malunion: In some cases, the bones may not fuse properly (nonunion), or they may heal in the wrong position (malunion), which may require additional surgery.
- Nerve Injury: Nearby nerves may be injured during surgery, leading to numbness, tingling, or weakness in the hand or wrist.
- Stiffness: While fusion eliminates pain, it also limits the range of motion at the affected joint, which can reduce flexibility.
- Hardware Complications: The screws, plates, or pins used to hold the bones together may cause irritation or complications, requiring their removal in some cases.
Conclusion
Arthritis surgery fusion (arthrodesis) is an effective treatment for severe arthritis in the hand and wrist, especially when other treatment options have failed. By fusing the bones of the affected joint, this procedure eliminates pain, stabilizes the joint, and prevents further deterioration. While the fusion limits joint movement, it can still provide significant improvements in hand or wrist function, allowing patients to return to daily activities without pain.
If you are suffering from arthritis in the hand or wrist and have not found relief through other treatments, consult with an orthopedic or hand surgeon to discuss whether arthritis surgery fusion is right for you. Proper post-surgical care and rehabilitation are essential for achieving the best possible outcome.
Shoulder Arthroscopy Surgery
Shoulder Arthroscopy Surgery: Overview, Indications, and Recovery
Shoulder arthroscopy is a minimally invasive surgical procedure used to diagnose and treat various shoulder conditions. During the procedure, a small camera (arthroscope) and specialized instruments are inserted through tiny incisions to visualize and repair issues within the shoulder joint.
Indications for Shoulder Arthroscopy Surgery
Shoulder arthroscopy may be recommended for several conditions, including:
- Rotator Cuff Tears: Tears of the rotator cuff tendons, often caused by trauma, overuse, or aging, may require surgical repair.
- Labral Tears: Tears in the labrum (e.g., SLAP tears) can cause pain and instability and may require arthroscopic repair.
- Shoulder Impingement: In cases where conservative treatments fail, arthroscopy can be used to remove bone spurs or smooth rough areas to reduce impingement.
- Shoulder Instability: Arthroscopy can be used to repair or tighten the ligaments and capsule in cases of shoulder dislocations or recurrent instability.
- Arthritis: In cases of severe shoulder arthritis, arthroscopy can be used for joint cleaning (debridement) or other procedures to relieve pain.
- Biceps Tendon Problems: Issues like biceps tendonitis or a torn biceps tendon may be addressed using arthroscopy.
Procedure for Shoulder Arthroscopy Surgery
Shoulder arthroscopy is typically performed under general anesthesia or regional anesthesia (e.g., a nerve block). The procedure involves:
- Incisions: Several small incisions are made around the shoulder joint. One incision is used to insert the arthroscope (camera), while others are used for specialized instruments.
- Visualization: The arthroscope is inserted to provide a clear view of the inside of the shoulder joint. The surgeon can then diagnose the issue and guide instruments to repair it.
- Repair: Depending on the condition, the surgeon may trim damaged tissue, remove bone spurs, repair torn tendons, or tighten ligaments.
- Closing: After the procedure is completed, the incisions are closed with stitches or adhesive strips.
Benefits of Shoulder Arthroscopy Surgery
- Minimally Invasive: Smaller incisions lead to less tissue damage, less pain, and a quicker recovery compared to traditional open surgery.
- Shorter Hospital Stay: Many patients can go home the same day, reducing the time spent in the hospital.
- Reduced Risk of Infection: Smaller incisions typically reduce the risk of infection and complications.
- Faster Recovery: Recovery time is generally quicker, with less scarring and muscle atrophy compared to open surgery.
Symptoms or Conditions Treated by Shoulder Arthroscopy Surgery
- Pain: Persistent shoulder pain, especially during overhead activities, that does not respond to conservative treatments.
- Weakness: Decreased strength or function in the shoulder, particularly in cases of tendon tears or instability.
- Limited Range of Motion: Difficulty moving the shoulder through its full range, especially with rotator cuff or labral injuries.
- Instability: A sensation of the shoulder “giving out,” often due to ligament or capsule damage.
Recovery and Rehabilitation After Shoulder Arthroscopy Surgery
Recovery from shoulder arthroscopy varies depending on the specific procedure performed, but typically includes:
- Initial Recovery:
- Rest and Immobilization: A sling or brace is typically worn for several weeks to support the shoulder while it heals.
- Pain Management: Ice therapy and prescribed medications (e.g., NSAIDs or narcotics) are used to manage pain.
- Physical Therapy:
- Range of Motion Exercises: Early rehabilitation focuses on restoring motion to the shoulder.
- Strengthening Exercises: As healing progresses, strengthening exercises are introduced to rebuild muscle strength and stability.
- Return to Activity: Athletes and active individuals typically return to sports or strenuous activities after 4–6 months, depending on the type of surgery.
- Long-Term Care:
- Full recovery from shoulder arthroscopy can take 3 to 6 months, with the shoulder reaching its maximum strength and function after rehabilitation.
Risks of Shoulder Arthroscopy Surgery
While shoulder arthroscopy is generally safe, some potential risks include:
- Infection: As with any surgical procedure, there is a risk of infection at the incision sites.
- Nerve or Blood Vessel Injury: Although rare, nearby nerves or blood vessels may be injured during the procedure.
- Stiffness or Scar Tissue Formation: Some patients may experience reduced range of motion or develop scar tissue that limits shoulder movement.
- Failure to Relieve Symptoms: In some cases, the surgery may not fully resolve the pain or dysfunction, requiring additional treatment or surgery.
Shoulder arthroscopy surgery is a highly effective option for treating many shoulder injuries, with faster recovery times compared to traditional surgery. Proper post-surgery rehabilitation is crucial for achieving the best outcomes and restoring full shoulder function.
Total Shoulder Arthroplasty
Total Shoulder Arthroplasty: Overview, Indications, and Recovery
Total shoulder arthroplasty (TSA), also known as shoulder replacement surgery, is a procedure in which the damaged parts of the shoulder joint are replaced with artificial components. It is typically performed to relieve pain and restore function in individuals with severe shoulder arthritis or other degenerative joint conditions.
Indications for Total Shoulder Arthroplasty
TSA may be recommended for several conditions, including:
- Osteoarthritis: Degenerative wear and tear of the shoulder joint that leads to pain, stiffness, and loss of motion.
- Rheumatoid Arthritis: An autoimmune disorder that can cause inflammation and damage to the shoulder joint.
- Rotator Cuff Arthropathy: A combination of rotator cuff tears and arthritis in the shoulder that leads to severe pain and dysfunction.
- Fractures: Severe fractures of the humeral head or shoulder that cannot be repaired with other surgical methods.
- Post-Traumatic Arthritis: Arthritis that develops after an injury or trauma to the shoulder joint.
Procedure for Total Shoulder Arthroplasty
Total shoulder arthroplasty is typically performed under general anesthesia or regional anesthesia (nerve block). The procedure involves:
- Incisions: A single incision is made over the front of the shoulder to access the joint.
- Removal of Damaged Tissue: The surgeon removes the damaged portions of the shoulder joint, including the worn-out cartilage from the glenoid (shoulder socket) and the head of the humerus (upper arm bone).
- Implantation of Prostheses: The damaged parts are replaced with artificial components:
- A prosthetic humeral head is attached to the top of the humerus.
- A prosthetic glenoid component is inserted into the shoulder socket.
- Reconstruction: In some cases, additional procedures, such as tendon repair or ligament tightening, may be performed.
- Closing: After the prostheses are in place, the incision is closed with stitches or staples, and a dressing is applied.
Benefits of Total Shoulder Arthroplasty
- Pain Relief: TSA is highly effective in alleviating chronic shoulder pain, especially from arthritis or fractures.
- Restoration of Function: The procedure improves shoulder function, allowing patients to perform daily activities more easily, including lifting and reaching overhead.
- Long-Term Solution: TSA provides a long-lasting solution for patients with severe shoulder joint damage that cannot be addressed by other methods.
Symptoms or Conditions Treated by Total Shoulder Arthroplasty
- Severe Shoulder Pain: Chronic pain that persists even with conservative treatments like physical therapy, medications, or injections.
- Stiffness: Limited range of motion in the shoulder joint, especially when trying to raise the arm or rotate the shoulder.
- Weakness: Difficulty lifting, reaching, or performing daily tasks due to joint damage.
- Instability: In cases of arthritis combined with rotator cuff dysfunction, the shoulder may feel unstable or prone to dislocations.
Recovery and Rehabilitation After Total Shoulder Arthroplasty
Recovery from total shoulder arthroplasty typically involves several phases, and full recovery can take several months:
- Initial Recovery:
- Rest and Immobilization: A sling is worn for the first 4–6 weeks to support the shoulder and allow the tissues to heal.
- Pain Management: Pain medications, ice therapy, and anti-inflammatory drugs are used to manage pain and swelling during the initial recovery period.
- Physical Therapy:
- Passive Range of Motion: Early physical therapy focuses on gentle exercises to regain range of motion, typically starting with passive movements where the therapist assists in moving the arm.
- Strengthening Exercises: As healing progresses, strengthening exercises are introduced to rebuild shoulder strength and function.
- Functional Activities: Gradual return to activities of daily living is encouraged as the shoulder regains mobility and strength.
- Long-Term Recovery:
- Full recovery from TSA can take 3 to 6 months, with some patients returning to normal activities, including light recreational sports, after 4–6 months.
- Ongoing therapy may be required for months to maximize function and maintain flexibility.
Risks of Total Shoulder Arthroplasty
While TSA is a safe and effective procedure, some risks include:
- Infection: As with any surgery, there is a risk of infection, especially at the surgical site.
- Blood Clots: Deep vein thrombosis (DVT) or pulmonary embolism (PE) may occur, especially in patients who are immobile for long periods.
- Implant Loosening or Wear: Over time, the artificial components may wear out or loosen, requiring revision surgery.
- Nerve or Blood Vessel Injury: There is a small risk of injury to nearby nerves or blood vessels during surgery.
- Stiffness or Reduced Range of Motion: In some cases, patients may experience limited movement post-surgery, particularly if rehabilitation is not followed properly.
- Dislocation: Though rare, dislocation of the prosthetic joint may occur, especially in the early post-operative period.
Total Shoulder Arthroplasty is a highly effective surgical option for patients suffering from severe shoulder pain and dysfunction due to arthritis, fractures, or other joint conditions. While recovery can take time, many patients experience significant improvements in pain relief and shoulder function, allowing them to return to daily activities and, in some cases, light recreational sports.
Reverse Total Shoulder Arthroplasty
Reverse Total Shoulder Arthroplasty: Overview, Indications, and Recovery
Reverse total shoulder arthroplasty (RTSA) is a surgical procedure designed to treat severe shoulder arthritis, rotator cuff arthropathy, or complex shoulder conditions where traditional shoulder replacement may not be effective. Unlike conventional shoulder replacement, RTSA involves reversing the anatomy of the shoulder joint, placing the ball on the socket side and the socket on the ball side to improve shoulder function, especially in cases with rotator cuff damage.
Indications for Reverse Total Shoulder Arthroplasty
RTSA may be recommended for several conditions, including:
- Rotator Cuff Arthropathy: Severe arthritis in the shoulder combined with a massive rotator cuff tear that cannot be repaired.
- Shoulder Osteoarthritis: Advanced arthritis in the shoulder, particularly in cases where the rotator cuff tendons are severely damaged or torn.
- Failed Shoulder Replacement: In some cases, if a traditional shoulder replacement fails, RTSA may be considered to improve pain relief and function.
- Fractures: Complex fractures of the humeral head or shoulder that cannot be repaired with traditional methods, especially in older individuals.
- Rheumatoid Arthritis: Advanced rheumatoid arthritis with associated rotator cuff damage.
Procedure for Reverse Total Shoulder Arthroplasty
Reverse total shoulder arthroplasty is typically performed under general anesthesia. The procedure involves:
- Incisions: A single incision is made at the front of the shoulder to access the joint.
- Removal of Damaged Tissue: The surgeon removes the damaged parts of the shoulder joint, including the arthritic bone and cartilage.
- Reversing the Joint: The main difference between traditional shoulder replacement and RTSA is that the components are reversed:
- A prosthetic socket is placed on the humeral head (the ball side).
- A prosthetic ball is placed on the glenoid (the socket side). This change in anatomy allows the deltoid muscle (instead of the rotator cuff) to compensate for the loss of shoulder function.
- Reconstruction: If necessary, the surgeon may also repair or reconstruct tendons and ligaments to improve stability.
- Closing: After the components are in place, the incision is closed with sutures or staples, and a dressing is applied.
Benefits of Reverse Total Shoulder Arthroplasty
- Improved Function: RTSA restores function in shoulders with severe rotator cuff damage, allowing the deltoid muscle to compensate for the loss of rotator cuff function.
- Pain Relief: RTSA is highly effective in alleviating chronic pain caused by arthritis, rotator cuff tears, or fractures.
- Restoration of Mobility: The procedure improves shoulder range of motion and allows patients to perform daily activities like lifting, reaching, and dressing.
- Increased Stability: The reversed components provide better stability in cases of rotator cuff deficiency, reducing the risk of dislocation.
Symptoms or Conditions Treated by Reverse Total Shoulder Arthroplasty
- Severe Shoulder Pain: Chronic pain, particularly from arthritis or rotator cuff tears, that persists despite conservative treatments like medication, physical therapy, or injections.
- Loss of Function: Difficulty lifting, reaching, or performing activities of daily living due to rotator cuff damage or arthritis.
- Instability: A sense of the shoulder “giving out” or instability, especially in cases of rotator cuff deficiency.
- Limited Range of Motion: Inability to move the shoulder fully, particularly with overhead or reaching motions.
Recovery and Rehabilitation After Reverse Total Shoulder Arthroplasty
Recovery after RTSA is similar to traditional shoulder replacement but may take a bit longer due to the complexity of the procedure. It typically involves several phases:
- Initial Recovery:
- Rest and Immobilization: A sling is worn for 4–6 weeks to protect the shoulder and allow healing.
- Pain Management: Ice therapy, anti-inflammatory medications, and prescribed pain medications are used to manage swelling and pain.
- Physical Therapy:
- Range of Motion: Physical therapy begins with gentle range of motion exercises to gradually increase flexibility and mobility.
- Strengthening: As healing progresses, the focus shifts to strengthening the shoulder and surrounding muscles, particularly the deltoid, to improve function.
- Functional Exercises: Patients work on regaining independence in daily activities such as dressing, lifting, and reaching.
- Long-Term Recovery:
- Full recovery typically takes 4–6 months, with patients returning to light activities around 3 months and full activities after 6 months.
- Ongoing physical therapy is essential to achieve optimal function and strength in the shoulder.
Risks of Reverse Total Shoulder Arthroplasty
While RTSA is a highly effective procedure, it carries some risks:
- Infection: As with any surgery, there is a risk of infection, especially at the surgical site.
- Blood Clots: Deep vein thrombosis (DVT) or pulmonary embolism (PE) may develop, particularly in patients who are immobile for long periods.
- Dislocation: There is a risk of the prosthetic components dislocating, especially early in the recovery phase.
- Implant Loosening: Over time, the prosthetic components may loosen or wear out, potentially requiring revision surgery.
- Nerve or Blood Vessel Injury: Rarely, nearby nerves or blood vessels can be damaged during surgery.
- Stiffness or Limited Motion: Some patients may experience stiffness or difficulty achieving full range of motion after the procedure.
Reverse Total Shoulder Arthroplasty is an excellent option for patients with severe shoulder arthritis or rotator cuff arthropathy, particularly when the rotator cuff is irreparably damaged. The procedure provides significant pain relief, restores shoulder function, and improves quality of life. Rehabilitation is critical to achieve the best possible outcomes and maximize shoulder mobility.
Shoulder Bracing
Shoulder Bracing: Types, Uses, and Benefits
Shoulder bracing refers to the use of a supportive device worn around the shoulder to stabilize the joint and prevent excessive movement. Braces are commonly used to treat a variety of shoulder injuries, such as dislocations, strains, sprains, or post-surgical recovery. They help reduce pain, provide support, and assist in the healing process by limiting movement and preventing further injury.
Indications for Shoulder Bracing
Shoulder bracing may be recommended for several conditions, including:
- Shoulder Instability: Following a shoulder dislocation or subluxation, a brace can help prevent the joint from moving out of place and reduce the risk of re-injury.
- Rotator Cuff Injuries: For partial tears or strains, a brace can limit movement and provide support while the injury heals.
- Post-Surgical Recovery: After shoulder surgeries, such as rotator cuff repairs or shoulder replacement, a brace can help protect the joint during recovery and allow for proper healing.
- Acromioclavicular (AC) Joint Injuries: For clavicle (collarbone) injuries, shoulder braces can provide stabilization and support during the healing process.
- Fractures: A brace is used to immobilize the shoulder after fractures or bone injuries, preventing unwanted movement and aiding the healing process.
- Arthritis: Shoulder braces can help alleviate discomfort caused by shoulder arthritis by supporting the joint and reducing strain.
Types of Shoulder Braces
There are different types of shoulder braces, each designed to address specific injuries and needs:
- Shoulder Immobilizers: These braces are designed to limit all motion in the shoulder joint. They are often used after surgery or following a dislocation to keep the shoulder in a neutral, non-moving position.
- Shoulder Slings: Often used for fractures or post-surgery, these slings keep the arm in place by suspending it at the side of the body, reducing strain on the shoulder joint and promoting healing.
- Shoulder Stabilizers: These braces provide moderate support and are typically used to help prevent re-injury in patients with shoulder instability or rotator cuff issues. They allow for some movement while still providing control and support to the joint.
- Clavicle Braces: Also known as figure-of-eight braces, these are designed to support and stabilize the collarbone (clavicle), particularly after fractures.
- Compression Sleeves: These are less restrictive and are used for mild shoulder injuries, such as strains or inflammation, providing compression to reduce swelling and discomfort.
Benefits of Shoulder Bracing
- Pain Relief: Braces help reduce shoulder pain by supporting the joint and preventing aggravating movements that could worsen the condition.
- Stabilization: They help stabilize the shoulder, reducing the risk of dislocation or further damage to the joint, especially in cases of instability or after surgery.
- Injury Prevention: For athletes or individuals involved in high-impact activities, shoulder braces can help prevent further injury to a previously damaged or weak shoulder joint.
- Facilitates Healing: By immobilizing the shoulder or limiting certain motions, braces allow soft tissues to heal and reduce the risk of re-injury during the recovery process.
- Enhanced Comfort: Shoulder braces can reduce swelling, provide compression, and improve comfort, allowing individuals to engage in daily activities with less pain.
Conditions or Symptoms Treated by Shoulder Bracing
- Shoulder Pain: For conditions like rotator cuff tears, arthritis, or tendonitis, braces can help alleviate pain and provide relief during movement.
- Shoulder Instability: Braces help stabilize the joint after dislocations or repeated subluxations, preventing further dislocations.
- Post-Surgical Recovery: After shoulder surgeries, bracing can protect the healing tissues, ensuring the joint is not stressed during rehabilitation.
- Fractures or Fracture Recovery: Bracing provides immobilization for fractured bones in the shoulder, aiding in the healing process.
- Strains and Sprains: Shoulder bracing is useful for sprains, strains, or soft tissue injuries that require support and protection while healing.
Recovery and Rehabilitation with Shoulder Bracing
The use of shoulder braces is often a part of a broader rehabilitation plan that may include physical therapy and pain management. The timeline for bracing varies depending on the condition being treated:
- Initial Recovery:
- The brace is worn consistently during the early recovery phase, typically for several weeks, depending on the severity of the injury or surgery.
- Pain management, including ice therapy and medications, is combined with bracing to ensure comfort.
- Physical Therapy:
- As healing progresses, physical therapy may be incorporated to restore strength and range of motion. The brace may be worn less frequently during this phase.
- Gradual reintroduction of shoulder movements is crucial to avoid stiffness or muscle atrophy.
- Weaning Off the Brace:
- Over time, the individual will gradually phase out the use of the brace as the shoulder regains strength and stability.
- The rehabilitation process will continue, focusing on improving functional movements and preventing re-injury.
Risks of Shoulder Bracing
While shoulder braces are generally safe, there are a few risks to consider:
- Skin Irritation: Prolonged use of shoulder braces can cause skin irritation or pressure sores, particularly if the brace is not fitted properly.
- Muscle Weakness: Extended use of an immobilizing brace may lead to muscle weakness or atrophy, as the shoulder muscles are not being used as much.
- Reduced Mobility: Wearing a brace can limit range of motion and flexibility, so it is essential to follow rehabilitation protocols to maintain joint mobility.
- Discomfort: If the brace is too tight or not properly adjusted, it may cause discomfort or impede circulation.
Shoulder Bracing is an effective treatment option for many shoulder injuries, offering support, stability, and pain relief. When used as part of a comprehensive rehabilitation plan, shoulder braces help promote healing and prevent further injury, making them essential for both short-term recovery and long-term shoulder health.
CT-Guided TSA & rTSA Implants
CT-Guided Total Shoulder Arthroplasty (TSA) and Reverse Total Shoulder Arthroplasty (rTSA) Implants: Overview, Benefits, and Stryker VIP System
CT-guided total shoulder arthroplasty (TSA) and reverse total shoulder arthroplasty (rTSA) represent advanced surgical techniques for shoulder joint replacement, combining computer-assisted navigation and imaging for precision and improved outcomes. These techniques are especially beneficial for patients with complex shoulder conditions, as they allow surgeons to plan and execute joint replacements with high accuracy, ensuring optimal alignment and implant placement.
The Stryker VIP system is a notable example of a cutting-edge implant used in both TSA and rTSA procedures. It offers a versatile, patient-specific approach to shoulder arthroplasty, helping improve surgical outcomes and recovery.
CT-Guided Total Shoulder Arthroplasty (TSA)
CT-guided TSA involves using preoperative computed tomography (CT) imaging to create a 3D model of the shoulder joint. This model helps the surgeon plan the placement of the implants and the precise removal of damaged tissue.
- Procedure:
- The CT scan provides detailed images of the shoulder joint, enabling the surgeon to assess the bone structure, soft tissue condition, and alignment.
- The system generates a 3D model, allowing for preoperative planning and intraoperative guidance.
- During surgery, the surgeon uses the CT-guided system to ensure accurate placement of the prosthetic components, reducing the likelihood of complications such as implant misalignment.
- Benefits:
- Precision: The CT-guided approach improves the precision of implant placement, reducing the risk of misalignment and improving long-term outcomes.
- Personalization: The preoperative CT scan can help design a personalized surgical plan tailored to the patient’s anatomy.
- Faster Recovery: Because of the enhanced accuracy and minimized tissue disruption, recovery times can be faster compared to traditional methods.
CT-Guided Reverse Total Shoulder Arthroplasty (rTSA)
In reverse total shoulder arthroplasty, the shoulder joint’s natural anatomy is reversed, with the ball placed on the socket side and the socket placed on the ball side. CT-guided rTSA allows for even greater precision in cases of rotator cuff deficiency, complex fractures, or shoulder arthritis.
- Procedure:
- The CT scan provides detailed 3D imaging to assess the shoulder’s unique structural issues, such as rotator cuff damage or deformities.
- The 3D model helps the surgeon plan the most effective approach to reverse the joint, ensuring optimal placement of the components.
- During surgery, the surgeon uses real-time guidance from the CT system to position the implant components accurately.
- Benefits:
- Improved Stability: rTSA can improve shoulder stability, especially for patients with rotator cuff tears. CT-guided placement ensures a more stable and functional result.
- Enhanced Precision: The technique minimizes the chances of complications such as component loosening or dislocation.
- Better Functional Outcomes: Patients can expect improved range of motion and reduced pain, especially for those with severe shoulder arthritis or rotator cuff damage.
Stryker VIP System for TSA and rTSA
The Stryker VIP (Variable Insert Position) system is a specialized implant used for both total and reverse shoulder arthroplasties. It is designed to improve the functional outcomes and longevity of shoulder replacements. The VIP system incorporates advanced technology to ensure better positioning of the components, reducing complications and improving recovery.
- Features of the Stryker VIP System:
- Customized Fit: The VIP system provides a more customized fit for the patient, adjusting for the individual’s anatomy and alignment needs.
- Stability and Mobility: The system is designed to improve both shoulder stability and mobility, especially in patients who have rotator cuff damage or arthritis.
- Biological Fixation: It focuses on biological fixation, ensuring that the components integrate well with the natural bone structure for better long-term durability.
- Modular Design: The system has a modular design, allowing for flexibility in component selection and alignment adjustments during surgery.
- Benefits of the Stryker VIP System:
- Enhanced Accuracy: CT-guided surgery and the VIP system work together to provide greater accuracy in implant placement, ensuring the components align correctly to improve joint function.
- Faster Recovery: By improving accuracy and reducing tissue disruption, the VIP system helps promote faster healing and quicker return to normal activities.
- Long-Term Results: The modular design and custom fitting lead to more durable and stable implants, reducing the need for revision surgeries.
Recovery and Rehabilitation after CT-Guided TSA or rTSA with Stryker VIP System
Recovery after a CT-guided shoulder replacement with a Stryker VIP system is similar to traditional shoulder replacement recovery but with potentially faster healing times and fewer complications due to the enhanced precision of the surgery.
- Initial Recovery:
- Patients are typically placed in a sling to immobilize the shoulder during the first few weeks of recovery.
- Pain management is addressed with medications and ice therapy to reduce swelling and discomfort.
- Physical Therapy:
- After the initial healing period, physical therapy is essential to restore shoulder strength and range of motion.
- A personalized rehabilitation plan is developed to help patients recover function quickly and reduce stiffness.
- Long-Term Recovery:
- Most patients can return to light activities after 3–6 months, with full recovery taking up to 12 months depending on the complexity of the surgery and rehabilitation progress.
Risks of CT-Guided TSA and rTSA with Stryker VIP System
Although CT-guided TSA and rTSA procedures with Stryker VIP implants offer many benefits, there are potential risks, including:
- Infection: As with any surgical procedure, there is a risk of infection, particularly if the implant is not properly placed or maintained.
- Implant Loosening: Though rare, implants may loosen over time, especially if not accurately placed or if the shoulder undergoes excessive stress post-surgery.
- Nerve or Vessel Injury: As with any shoulder surgery, there is a risk of damaging surrounding nerves or blood vessels.
- Dislocation: There is always a small risk of dislocation, particularly in the early stages of recovery, before the surrounding muscles and tissues are fully healed.
- Stiffness or Reduced Range of Motion: Some patients may experience stiffness or limited motion if the rehabilitation process is not followed correctly.
CT-guided TSA and rTSA with Stryker VIP System are advanced surgical techniques that combine precision imaging and customized implants to optimize shoulder replacement outcomes. With improved accuracy, personalized treatment, and better functional results, these procedures offer significant advantages for patients with complex shoulder conditions, helping them recover faster and with fewer complications.


